DCMC ER Convenience A Streamlined Experience
DCMC adds a dose of convenience for its ER patients, streamlining the experience for those seeking urgent care. This initiative focuses on improving check-in, reducing wait times, and enhancing communication, all aiming to make the ER visit less stressful and more efficient. The changes include streamlined processes and new technologies, leading to significant improvements in patient satisfaction and operational efficiency.
A comparison of before and after processes highlights the tangible benefits for patients.
This article delves into the specifics of these improvements, examining the impact on patient satisfaction, operational efficiency, and cost savings. We’ll also compare DCMC’s approach with similar initiatives in other healthcare systems, exploring potential future trends and challenges.
Introduction to DCMC’s Convenience for ER Patients
DCMC is committed to enhancing the patient experience in its emergency room (ER). Recognizing the often stressful nature of seeking emergency care, DCMC has implemented various initiatives aimed at streamlining processes and improving communication, ultimately leading to a more comfortable and efficient experience for all patients. These improvements range from digital check-in options to enhanced communication channels.DCMC’s dedication to patient comfort extends beyond simply addressing immediate medical needs.
The goal is to create a supportive and informative environment, reducing anxiety and improving the overall quality of care received during a critical time. This focus on patient convenience is reflected in the dedicated efforts to optimize every stage of the ER visit.
Streamlined Check-in Processes, Dcmc adds a dose of convenience for its er patients
DCMC has introduced a digital check-in system that allows patients to register online before arriving at the hospital. This pre-registration process significantly reduces wait times at the front desk. Patients can complete necessary paperwork and provide medical history information ahead of time, ensuring a smoother and faster check-in experience upon arrival. This online pre-registration minimizes delays and allows staff to focus on patient care immediately upon arrival.
Reduced Waiting Times
To further optimize patient flow, DCMC has implemented a sophisticated system for triaging patients based on the severity of their conditions. This prioritization system ensures that patients with critical needs receive immediate attention, while less urgent cases are managed in a timely manner. This system helps manage the patient load more effectively, reducing the overall wait time for all patients.
Improved Communication
DCMC has established clear communication channels between patients, their families, and medical staff. This includes providing real-time updates on patient status through a dedicated app or SMS messages. Patients can also access their medical records electronically, enabling them to stay informed about their care. This transparent communication minimizes anxiety and keeps patients and their loved ones well-informed during a potentially stressful situation.
Comparison of Patient Experience
| Feature | Before | After |
|---|---|---|
| Check-in time | Often lengthy wait at the front desk, filling out paperwork in person. | Pre-registration online, expedited check-in upon arrival. |
| Waiting time | Potentially long wait times, depending on patient volume and severity of conditions. Limited communication updates. | Triaged based on severity; updated on status via app/SMS. Improved flow management. |
| Communication | Limited communication; patients and families may be left uncertain about their loved one’s status. | Real-time updates via app or SMS, access to medical records. |
Impact on Patient Satisfaction: Dcmc Adds A Dose Of Convenience For Its Er Patients
DCMC’s initiatives aimed at enhancing emergency room (ER) patient convenience are poised to significantly impact patient satisfaction scores. Improved efficiency and streamlined processes can directly translate into a more positive patient experience, leading to higher levels of satisfaction and potentially improved feedback. Understanding how these improvements affect patient perception is crucial for evaluating the success of the initiatives and identifying areas for future enhancement.
Potential Positive Effects on Patient Satisfaction Scores
The enhanced convenience measures implemented at DCMC, such as expedited check-in procedures and improved wait times, are expected to lead to a substantial increase in patient satisfaction. Patients who experience a smooth and efficient journey through the ER are more likely to feel valued and respected. This positive perception directly correlates with higher satisfaction scores. Furthermore, reduced wait times can mitigate stress and anxiety, contributing to a more favorable overall experience.
The improved flow of patients through the ER, resulting from these enhancements, is projected to have a significant impact on the patient experience, thus directly influencing patient satisfaction scores.
Patient Feedback Measurement Metrics
Measuring patient satisfaction in the ER involves utilizing various metrics and survey questions. Standardized questionnaires, often employing Likert scales, are common tools for gauging patient perceptions across various aspects of the ER experience. These scales often evaluate aspects such as the speed and efficiency of check-in, the length of wait times, the helpfulness and courtesy of staff, and the overall cleanliness and comfort of the environment.
Specific questions might include ratings on the helpfulness of staff, the ease of navigation within the facility, and the overall experience.
Examples of Survey Questions
- How would you rate the overall efficiency of your check-in process? (Excellent, Good, Fair, Poor)
- How would you rate the length of your wait time? (Much too long, Too long, Acceptable, Too short, Much too short)
- How would you rate the helpfulness and courtesy of the staff you encountered? (Very helpful, Helpful, Neutral, Unhelpful, Very unhelpful)
- How would you rate the cleanliness and comfort of the waiting area? (Excellent, Good, Fair, Poor)
- Would you recommend DCMC’s ER to others? (Yes, No, Maybe)
Potential Areas for Further Improvement
While the implemented initiatives show promise, potential areas for further improvement include:
- Communication: Enhancing communication regarding wait times and estimated wait times, providing updates to patients throughout the process, and using clear signage can greatly enhance the patient experience.
- Patient Education: Implementing educational materials within the waiting area can help patients understand the process, reduce anxiety, and provide an additional layer of information about procedures.
- Staff Training: Ongoing training for staff on communication techniques, empathy, and patient-centered care can significantly impact the interactions patients have with staff, creating a more positive atmosphere.
Positive and Negative Feedback on ER Patient Experiences
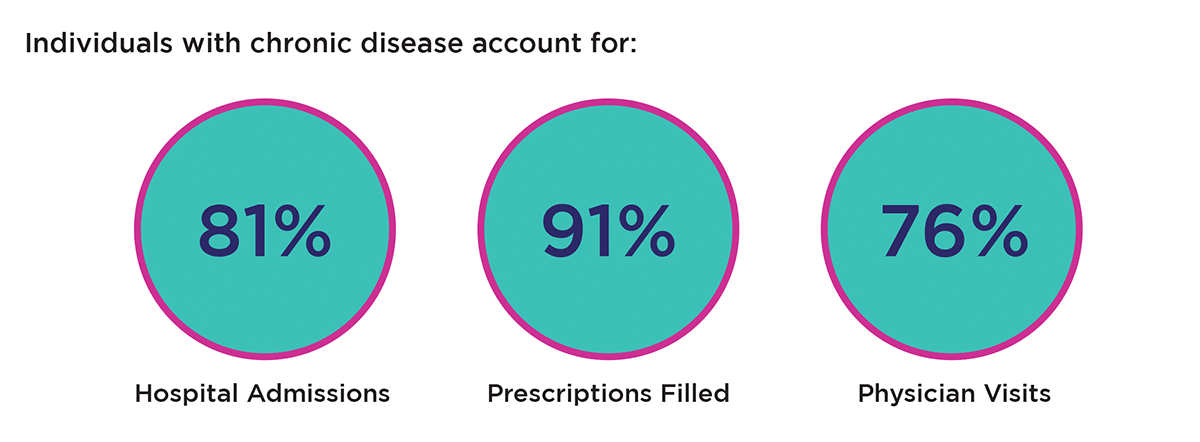
Operational Efficiency and Cost Savings
Streamlining emergency room operations at DCMC promises significant improvements in efficiency and cost savings. By optimizing workflows and implementing technology, DCMC can reduce wait times, decrease administrative burdens, and ultimately, deliver more efficient and affordable care. This translates to a better patient experience and enhanced financial sustainability for the hospital.The implementation of these initiatives is expected to result in substantial cost reductions across various operational aspects of the emergency room, while simultaneously improving patient care.
This includes optimized staffing allocation, streamlined supply management, and a more efficient patient flow. The shift from the previous model to the new model promises a more responsive and cost-effective service.
Impact on Operational Efficiency
DCMC’s new ER initiatives are designed to dramatically improve operational efficiency by reducing bottlenecks and streamlining processes. By implementing a new patient intake system, the hospital anticipates a significant reduction in wait times for triage and initial assessments. This will involve leveraging technology for quicker data entry and automated scheduling. The new system will allow for real-time monitoring of patient flow, enabling proactive adjustments to resource allocation, further improving efficiency.
Potential Cost Savings
The improved operational efficiency is expected to translate into substantial cost savings for DCMC. Reduced wait times directly translate into decreased staff overtime and improved utilization of resources. By optimizing supply chain management, and using data-driven insights, DCMC can identify and minimize unnecessary expenses. This will improve the bottom line and allow for greater investment in patient care.
Detailed Analysis of Workflow Improvements
The previous ER workflow often involved lengthy wait times due to manual processes and insufficient capacity for handling peak loads. The new workflow, illustrated below, leverages technology and improved resource allocation for a more streamlined patient journey.
(Diagram would visually illustrate the difference between the previous and new ER workflows. The previous workflow would depict a convoluted path with multiple handoffs and delays. The new workflow would show a more direct and streamlined process, utilizing technology for data entry and automated scheduling, and incorporating real-time monitoring to optimize staffing and resource allocation. )
Projected Cost Savings
The following table Artikels the anticipated cost savings resulting from the implementation of DCMC’s improved ER processes:
| Area | Previous Cost | New Cost | Savings |
|---|---|---|---|
| Staff Time (Overtime) | $15,000 per month | $5,000 per month | $10,000 per month |
| Supplies (Wasted/Expired) | $2,500 per month | $500 per month | $2,000 per month |
| Administrative Costs (Data Entry Errors) | $1,000 per month | $0 | $1,000 per month |
| Total Savings | $13,500 per month |
Comparison with Other Healthcare Systems
Examining DCMC’s Emergency Room (ER) convenience initiatives reveals a critical need to understand their effectiveness within a broader healthcare context. Comparing DCMC’s approach with similar initiatives in other systems offers valuable insights into best practices and potential areas for improvement. This comparison helps identify strengths and weaknesses, ultimately contributing to enhanced patient care and operational efficiency.A thorough evaluation of existing ER convenience programs in other healthcare systems is essential.
This analysis allows for a critical assessment of the effectiveness and implementation strategies of these initiatives, offering a framework for evaluating DCMC’s strategies. Analyzing successful and unsuccessful implementations provides valuable lessons for optimization and improvement.
Technology Use in Other Systems
Various healthcare systems are leveraging technology to enhance ER patient experience and operational efficiency. Remote patient monitoring, telehealth consultations, and online appointment scheduling are becoming increasingly common. For instance, some systems utilize AI-powered triage tools to prioritize patient needs, reducing wait times and improving resource allocation. Other systems have implemented sophisticated electronic health record (EHR) systems that streamline communication and information sharing among staff, leading to faster diagnoses and treatments.
DCMC’s focus on digital platforms, like online check-in and appointment scheduling, aligns with these trends.
DCMC’s new ER improvements are a real game-changer, adding a much-needed dose of convenience for patients. It’s all about streamlining the process, and that’s a huge plus. This echoes the important work being done by groups like sustaining our waters the fox wolf watershed alliance , who are dedicated to protecting our natural resources. Ultimately, both initiatives contribute to better outcomes, for both human health and environmental well-being, and that’s something we can all get behind.
Staff Training and Patient Education
Effective implementation of convenience initiatives requires comprehensive staff training. Other healthcare systems often employ standardized training programs focusing on communication skills, empathy, and the use of new technologies. These programs aim to ensure consistent and high-quality patient interactions. Furthermore, robust patient education programs, both pre- and post-visit, are crucial for effective communication and adherence to treatment plans.
Patient portals and educational materials are often used to provide patients with information about their conditions, medications, and follow-up appointments.
Comparison Table: DCMC vs. Other Systems
| Feature | DCMC | Other Systems |
|---|---|---|
| Technology Use | Utilizes online check-in, appointment scheduling, and streamlined digital communication channels. | Many utilize AI-powered triage, telehealth consultations, and sophisticated EHR systems for enhanced efficiency and communication. Some use wearable technology for remote monitoring. |
| Staff Training | Focuses on training staff in using new technologies and providing exceptional patient service. | Employ standardized training programs emphasizing communication skills, empathy, and use of advanced technologies, often including simulation exercises for critical situations. Continuous training on best practices is common. |
| Patient Communication | Emphasizes clear communication channels and patient portals for appointment reminders and updates. | Many offer diverse communication options, including mobile apps for appointment reminders, progress updates, and medication management. Interactive patient portals are often integrated into the overall system. |
| Patient Feedback | Collects patient feedback through surveys and direct interactions. | Actively seek feedback through surveys, patient satisfaction questionnaires, and feedback forms, analyzing data to identify areas for improvement and adjust services accordingly. Some utilize focus groups to gain deeper insights. |
Examples of Successful and Unsuccessful Implementations
Successful implementations often involve a phased approach, starting with a pilot program in a specific area or department. This allows for adjustments and refinement before widespread adoption. Furthermore, strong leadership support and consistent communication throughout the organization are vital for success. Conversely, rushed implementations without proper training or clear communication can lead to confusion and frustration among staff and patients.
A lack of patient engagement and feedback mechanisms can also hinder success.
DCMC’s new ER improvements are a welcome boost for patients, adding a much-needed dose of convenience. Think about how innovations in energy production are also looking at alternative materials, like those explored in the future of sustainable energy looks to alternative materials , for more efficient and eco-friendly solutions. Ultimately, these advancements, like the improved ER experience, highlight the drive for progress and better outcomes in various sectors.
Future Trends and Projections
The Emergency Room (ER) landscape is constantly evolving, driven by technological advancements and changing patient expectations. Predicting future trends requires understanding the current momentum and anticipating how technology and societal shifts will shape the patient experience. DCMC’s current initiatives offer a strong foundation for adapting to these changes, but foresight is critical to maximizing their long-term impact.
Future Trends in ER Patient Convenience
The future of ER patient convenience will likely center on proactive care, streamlined processes, and personalized experiences. Telemedicine and remote monitoring will play an increasingly significant role in enabling patients to access care before needing an ER visit, potentially reducing the burden on the ER. This trend is already visible in other healthcare sectors, with companies like Teladoc and others offering virtual consultations and remote monitoring tools.
Simultaneously, patients will demand more sophisticated ways to schedule appointments, receive updates, and access their medical records digitally. The focus will remain on making the ER experience efficient, transparent, and less stressful.
Emerging Technologies Enhancing Patient Experience
Several emerging technologies promise to significantly enhance the patient experience in the ER. Artificial intelligence (AI) can be used to triage patients more effectively, potentially reducing wait times and ensuring the right patients receive immediate attention. AI-powered chatbots can also provide preliminary support, answer questions, and guide patients through the process. Real-time data visualization dashboards can provide staff with critical information about patient flow, resource availability, and potential bottlenecks, leading to better resource allocation and more efficient operations.
DCMC’s recent improvements to their ER, adding a dose of convenience for patients, is fantastic news. It’s great to see hospitals prioritizing patient experience, especially when considering the redesignation of the Stevens Points Breast Care Center, which received high marks in their recent review process. This streamlined approach at the ER aligns perfectly with the focus on comprehensive healthcare, and ultimately benefits the whole community, mirroring the dedication of facilities like the Stevens Points Breast Care Center in providing top-notch care.
Long-Term Impact of DCMC’s Initiatives
DCMC’s current initiatives, if sustained and expanded upon, have the potential to create a truly transformative impact on the patient experience in the long run. By focusing on technology adoption, streamlined processes, and personalized care, DCMC can create a more efficient and user-friendly ER environment. This could lead to improved patient satisfaction, reduced wait times, and better outcomes.
Potential Future Improvements for ER Patient Experiences
To further enhance the ER patient experience, DCMC should consider these potential improvements:
- Enhanced Telehealth Integration: Expanding telehealth capabilities to include virtual consultations, remote monitoring, and pre-ER symptom assessments will significantly reduce unnecessary ER visits and allow patients to receive care in a more convenient and timely manner. This could potentially reduce strain on the ER, as patients can receive preliminary assessment and treatment via telehealth platforms.
- AI-Powered Triage Systems: Implementing AI-powered triage systems can further optimize patient flow. This system will analyze patient data, including symptoms, medical history, and vital signs, to determine the urgency of their needs. This can help in faster identification of critical cases and reduce wait times for less urgent cases.
- Personalized Patient Portals: Creating a comprehensive patient portal that allows patients to access their medical records, schedule appointments, receive updates, and communicate with staff will empower patients and enhance their experience. Such portals can allow patients to track their progress and ensure timely communication with staff.
- Predictive Analytics for Resource Management: Implementing predictive analytics to anticipate potential resource bottlenecks (staffing, equipment) can optimize resource allocation, reducing wait times and ensuring smooth operations. This would involve real-time monitoring and forecasting to avoid shortages and delays.
Visual Representation of Technological Advancements
Imagine a streamlined, interactive dashboard (see below). This dashboard displays real-time data on patient flow, resource availability, and potential bottlenecks. Color-coded indicators highlight areas requiring attention, such as high patient volume in specific departments or equipment malfunctions. This visualization allows staff to proactively address potential issues, optimizing the overall ER experience.
| Category | Data Displayed | Impact |
|---|---|---|
| Patient Flow | Number of patients in each stage (arrival, triage, assessment, treatment), wait times | Identify bottlenecks and adjust staffing/resource allocation |
| Resource Availability | Beds, equipment, staff availability, medication levels | Prevent shortages and delays, optimize resource utilization |
| Potential Issues | Predictive alerts for potential issues, such as high patient volume or equipment malfunctions | Allow proactive interventions to maintain smooth operations |
Potential Challenges and Mitigation Strategies
Implementing enhanced convenience initiatives in the Emergency Room (ER) presents several potential hurdles. These challenges, ranging from technological integration to staff adaptation, must be proactively addressed to ensure the successful rollout and long-term sustainability of improved patient experiences. Careful planning and proactive mitigation strategies are crucial for minimizing disruptions and maximizing the benefits of these advancements.
Technological Integration Challenges
Integrating new technologies, such as advanced scheduling systems or telehealth platforms, into existing ER workflows can be complex. Compatibility issues with existing infrastructure, training requirements for staff, and potential glitches in software functionality are all potential obstacles. Moreover, ensuring data security and patient privacy in the context of new systems is paramount. Smooth transitions require careful planning and robust testing.
Staff Training and Support
Effective staff training is essential for successful implementation. Training programs should equip personnel with the skills and knowledge needed to operate new technologies and procedures, while also addressing potential anxieties or concerns. Adequate resources, including ongoing support and mentorship, are critical to fostering a positive learning environment. Staff buy-in and collaboration are vital for successful adoption of new processes.
Regular feedback sessions and opportunities for staff to share their experiences can contribute to refining the system.
Potential Patient Flow Disruptions
Introducing new procedures or systems might temporarily disrupt the existing flow of patients in the ER. Overcrowding, longer wait times, or misallocation of resources are possible consequences if not anticipated and addressed. Implementing buffer mechanisms, such as additional staff or re-routing strategies, can mitigate these issues. Clear communication with patients about potential delays and alternative options is essential.
Contingency Planning for Patient Convenience Issues
Developing a contingency plan for resolving issues related to patient convenience is critical. This plan should Artikel specific procedures for handling unexpected circumstances, such as system failures, staff shortages, or unforeseen patient volume fluctuations. A well-defined escalation protocol, backup resources, and clear communication channels are crucial components. Regular review and updates to the contingency plan are essential to ensure its effectiveness in addressing potential challenges.
For instance, a system that automatically prioritizes patients based on severity, with backup staff ready to assist, can ensure smooth operation even during high-volume periods.
Addressing Data Security Concerns
Ensuring the security and privacy of patient data is paramount. Implementing robust data encryption, access controls, and regular security audits are critical to protecting sensitive information. Adherence to relevant privacy regulations (e.g., HIPAA) is mandatory. This includes regular security training for all staff members involved in patient data handling, to ensure compliance and to minimize potential vulnerabilities.
Data breaches can have severe consequences, impacting both patients and the institution’s reputation. Robust security measures are not just a precaution, but a fundamental responsibility.
Closing Notes

In conclusion, DCMC’s commitment to enhancing ER patient convenience is a valuable step towards a more patient-centric healthcare model. The initiatives described in this article, from streamlined check-in procedures to improved communication channels, aim to make a tangible difference in patient experience. While challenges may arise, the potential benefits in patient satisfaction, operational efficiency, and cost savings suggest that these changes will positively impact the overall healthcare delivery system.
Future trends and projections indicate the potential for even greater improvements, making the ER visit a more positive and productive experience.