60 Years of Independent Private Practice Care
60 years of offering independent private practice care has shaped the landscape of healthcare, influencing patient experiences, professional development, and the financial models used by practitioners. This journey has been marked by significant societal and economic shifts, technological advancements, and evolving patient expectations. The narrative explores the historical context, patient journeys, professional growth, financial aspects, community impact, and future trends within this unique practice model.
From the early days to today, independent practitioners have adapted to meet the needs of their patients and communities, navigating challenges and seizing opportunities along the way. This exploration delves into the diverse experiences across different specialties and geographic regions, highlighting the resilience and adaptability of this vital segment of the healthcare industry.
Historical Significance
Sixty years of independent private practice care has witnessed profound transformations. This period has seen significant shifts in healthcare delivery, driven by evolving societal needs, economic pressures, and technological advancements. From the rise of managed care to the emergence of telehealth, the landscape of independent practice has been reshaped continuously. Understanding this evolution is crucial for appreciating the challenges and opportunities faced by independent practitioners today.The structure and availability of independent private practice have been profoundly influenced by the societal and economic environment.
Changing demographics, insurance coverage, and patient expectations have all played a critical role in shaping the way independent practitioners operate. The ability of private practitioners to adapt to these shifts has been critical to their continued success.
Key Developments and Trends
Independent private practice care has undergone substantial evolution over the past six decades. The rise of managed care in the 1980s and 1990s, for example, introduced new reimbursement models and regulations that impacted the financial viability of private practices. This period also saw the growing importance of specialization and sub-specialization, leading to increased complexity in practice models. The introduction of electronic health records (EHRs) and advancements in telemedicine have further reshaped the way independent practitioners deliver care.
These changes have required significant adaptation and investment in technology and training.
Societal and Economic Factors
Several societal and economic factors have influenced the evolution of independent private practice. The changing demographics of the population, including increasing life expectancy and the growing prevalence of chronic diseases, have created new demands on healthcare services. The shift towards a more consumer-driven healthcare system, where patients actively participate in their care decisions, has also impacted the role of independent practitioners.
Economic factors, such as fluctuating insurance premiums, reimbursement rates, and the cost of healthcare services, have also shaped the landscape.
Challenges and Opportunities
Independent practitioners have faced numerous challenges throughout this period. Competition from larger healthcare organizations, the increasing complexity of regulations, and the need to adapt to technological advancements have been significant hurdles. However, these challenges have also presented opportunities for innovation and differentiation. The ability of independent practitioners to leverage their flexibility and personalized approach to care has proven valuable in a rapidly evolving healthcare environment.
Building strong patient relationships and establishing a niche within the market have been key strategies for success.
Geographic Variations
The practice of independent private care has varied significantly across different geographic regions. Factors such as the availability of healthcare resources, the prevalence of specific diseases, and the local economic conditions have all influenced the types of services offered and the challenges faced by independent practitioners. For instance, rural areas often face unique challenges in recruiting and retaining specialists, while urban areas might be more competitive due to a higher concentration of healthcare providers.
Timeline of Significant Events
- 1960s-1970s: The foundation of independent practice was established. The focus was primarily on primary care and general practice. Reimbursement structures were simpler compared to later periods.
- 1980s-1990s: The rise of managed care introduced new reimbursement models and regulations, impacting financial sustainability. Specialization and sub-specialization gained prominence.
- 2000s-2010s: The proliferation of electronic health records (EHRs) and the emergence of telehealth dramatically reshaped the delivery of care. Patient expectations for convenience and access increased.
- 2010s-Present: Continued emphasis on patient-centered care and value-based care models. The challenges of maintaining financial viability and adapting to new regulations remain prominent.
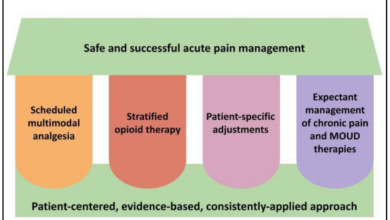
Patient Experience

For 60 years, the patient journey in independent private practice has been deeply intertwined with the evolving needs and expectations of our communities. This journey reflects not only the advancements in medical knowledge and technology, but also the changing social landscape and patient values. We’ve witnessed a remarkable transformation in how patients interact with their care providers, a transformation driven by the unwavering commitment to providing personalized, high-quality care within our practices.The patient experience in independent private practice has always been characterized by a focus on personalized care.
This has been particularly crucial in fostering trust and rapport, as evidenced by the longevity of many patient-physician relationships spanning decades. The approach emphasizes a holistic understanding of the patient, extending beyond the immediate medical concern to address their overall well-being.
Evolution of Patient Expectations
Patient expectations have significantly evolved over the past six decades. Initial expectations revolved primarily around access to quality medical care and competent diagnoses. The introduction of advanced diagnostic tools and treatments expanded patient expectations to include access to cutting-edge technologies, leading to more informed decision-making. Moreover, patients increasingly value proactive care and preventative measures. They want to be actively involved in their health management, seeking personalized treatment plans and a deeper understanding of their conditions.
Role of Technology in Shaping Patient Experience
Technology has undeniably revolutionized the patient experience. Initial interactions involved primarily in-person appointments and paper-based records. Now, patients often utilize online portals for scheduling, accessing medical records, communicating with their providers, and managing their health information. Telemedicine has further expanded access to care, especially for patients in remote areas or with mobility limitations. This integration of technology allows for more efficient and convenient access to information and care, while maintaining the personal touch of a dedicated provider.
Patient Experience Across Specialties
The patient experience can vary across specialties within independent private practice. For instance, patients seeking dermatological care may value a more aesthetically-focused approach and personalized skincare advice. Conversely, patients requiring cardiology services may prioritize advanced diagnostic tools and treatment protocols. The specific needs and preferences of each specialty influence the experience. However, a common thread remains: the desire for compassionate, evidence-based care delivered by experienced and knowledgeable professionals.
Building Trust and Rapport
Building trust and rapport with patients is paramount in independent private practice. This is achieved through active listening, clear communication, empathy, and a genuine concern for the patient’s well-being. Transparent and honest discussions about treatment options and potential risks are essential. The establishment of open communication channels, whether through regular check-ins or readily available contact information, reinforces the relationship.
Additionally, providers prioritize a calm and reassuring demeanor to create a safe and comfortable environment for patients to discuss their concerns.
Sixty years of offering independent private practice care is a testament to our commitment to providing personalized service. This longevity is built on a foundation of trust, which directly connects to the idea that authenticity is essential to brand building. Authenticity is essential to brand building because it fosters genuine connections with patients, and ultimately strengthens our reputation.
That same commitment to authenticity is what has helped us maintain a thriving practice for six decades.
Professional Development
For six decades, independent practitioners have navigated a dynamic landscape of evolving standards, technologies, and patient needs. This evolution has demanded continuous professional development, shaping the very fabric of private practice. Adapting to these changes has been crucial for maintaining high-quality care and ethical practice.The path of independent practice has been paved with both exciting opportunities and significant challenges.
Practitioners have had to constantly refine their skills, embrace new knowledge, and adapt to regulatory changes to maintain their professional relevance and credibility. The need for ongoing education has been paramount in maintaining competency and ensuring patient safety.
Evolving Professional Development Opportunities
The availability and accessibility of professional development opportunities have significantly expanded over the past 60 years. Early on, practitioners relied primarily on in-person workshops and seminars, often localized and less frequent. Today, online courses, webinars, and virtual conferences offer unparalleled flexibility and reach. This expanded access allows practitioners to engage in continuing education at their convenience, regardless of location.
Specialization has also become more accessible, with programs offering advanced training in specific areas like mindfulness, trauma-informed care, or cognitive behavioral therapy.
Continuing Education and Specialization
Continuing education is no longer a luxury but a necessity for maintaining competence in independent practice. The sheer volume of new research, therapeutic modalities, and technological advancements necessitates ongoing learning. Specialization has also become a key factor in attracting and retaining clients. By focusing on a particular area of expertise, practitioners can develop specialized knowledge and offer tailored treatment approaches, leading to improved outcomes for their patients.
Impact of Evolving Standards and Regulations
The regulatory landscape surrounding independent practice has undergone substantial changes over the past six decades. Initially, regulations focused primarily on licensing and credentialing. Now, there’s a greater emphasis on ethical conduct, data privacy, and patient safety. The implementation of HIPAA, for instance, has profoundly impacted how practitioners handle patient information. Furthermore, evolving ethical guidelines and best practices have reshaped the professional expectations and responsibilities of independent practitioners.
Sixty years of providing independent private practice care is a testament to dedication and hard work. Thinking about transitioning ownership? Knowing the right five tips for selling a business, like those outlined in this helpful guide five tips for selling a business , is crucial for a smooth and successful sale. This long-standing practice will continue to provide exceptional care for years to come.
Key Qualities and Skills for Success
Several key qualities and skills have proven crucial for success in independent practice throughout these six decades. Strong communication skills, both verbal and written, remain paramount for building rapport with patients and collaborating with colleagues. Adaptability and a willingness to embrace new technologies and approaches are essential for navigating the ever-changing landscape of healthcare. Furthermore, strong business acumen and financial management skills are critical for independent practitioners to effectively run their own practices.
Certifications and Licensures in Independent Practice
The requirements for certifications and licensures have evolved considerably over the past six decades. Initially, many practitioners relied on general licensing. The rise of specialization, however, has led to a more intricate web of certifications and licensures. These changes reflect the growing complexity and specialization within the field.
Financial Aspects
For 60 years, independent practitioners have navigated a complex financial landscape, adapting to evolving reimbursement models, regulatory changes, and technological advancements. This journey reflects the resilience and ingenuity of the private practice community, constantly seeking to balance the needs of patients with the financial sustainability of their businesses. Their success is a testament to their ability to adapt and innovate.Independent practitioners have often relied on a mix of strategies to ensure financial stability.
These strategies, from careful budgeting to seeking appropriate funding and using diverse payment methods, have been crucial for long-term survival and success.
Financial Strategies and Models
Independent practices have employed various financial strategies. Many have started with a focus on providing high-quality, personalized care, recognizing that this approach attracts patients and fosters loyalty. Building a strong reputation and establishing trust with clients has often been a primary driver of success. Careful cost management and efficient operations have also been crucial for maintaining profitability, and many have diversified their services to reduce reliance on a single source of income.
Financial Pressures and Support Systems
Independent practitioners face unique financial pressures. Fluctuating insurance reimbursements, administrative costs, and the need for continuous professional development can strain resources. Many have relied on support networks, such as mentorship programs, peer groups, and professional organizations, to navigate these challenges. Access to financial planning and consulting services has also been vital for making sound financial decisions. In recent years, there has been an increase in the availability of financial resources and coaching programs designed specifically for independent healthcare providers.
Evolution of Reimbursement Models, 60 years of offering independent private practice care
Reimbursement models have undergone significant changes over the past 60 years. The shift from fee-for-service to value-based care has presented both opportunities and challenges. Independent practitioners have had to adapt to these evolving models by focusing on outcome-based metrics and streamlining administrative processes. Understanding and effectively navigating the complexities of new payment structures is essential for long-term sustainability.
This has involved a shift from simply billing for services rendered to demonstrating the value of care provided.
Regulatory Changes and Technological Advancements
Regulatory changes, such as new regulations and standards, have impacted independent practices. These changes often involve additional administrative burdens and compliance costs. Technology has also played a transformative role, streamlining administrative tasks but requiring significant investments in software and training. The ability to adapt to new technologies and integrate them into existing practice workflows has been crucial.
Comparison of Billing and Payment Methods
Community Impact: 60 Years Of Offering Independent Private Practice Care

For sixty years, our independent practice has been deeply intertwined with the fabric of our local community. We’ve witnessed firsthand the evolving needs and aspirations of our patients, and we’ve strived to adapt our services to meet those changing demands. Our commitment to community well-being has extended beyond the clinical setting, encompassing active participation in local health initiatives and fostering a supportive environment for all.Our dedication to the community isn’t just about providing exceptional patient care; it’s about building relationships and becoming a vital part of the local ecosystem.
We’ve consistently sought ways to contribute to the overall health and prosperity of the communities we serve, from supporting local charities to collaborating with community health organizations.
Role of Independent Practice in Local Community
Independent practices have played a crucial role in shaping the local healthcare landscape over the past six decades. They’ve often been the first point of contact for individuals seeking medical care, particularly in underserved areas, and they’ve offered a level of personalized attention that larger healthcare systems sometimes struggle to replicate.
Examples of Supporting Community Health Initiatives
Our practitioners have actively participated in various community health initiatives. This includes volunteering time at local health fairs, offering free health screenings, and collaborating with schools to promote healthy lifestyle choices. For instance, our practice has partnered with the local YMCA to offer discounted health assessments and wellness workshops to the community. Furthermore, we have supported local food banks by providing free health consultations to their clients, recognizing the critical link between food security and overall health.
Impact on Access to Care in Diverse Communities
Independent practices have been instrumental in ensuring access to care for diverse communities. They have often established relationships with community leaders and organizations to understand the specific health needs of different populations and tailored their services accordingly. This personalized approach has proven vital in addressing health disparities and fostering trust within various cultural groups.
Evolving Relationship with Larger Healthcare Systems
The relationship between independent practices and larger healthcare systems has evolved significantly over the years. Initially, there was often a degree of independence and competition. However, in recent decades, we’ve seen a growing trend toward collaboration and partnership. This has taken the form of joint ventures for specialized services, shared resources, and referral networks that aim to enhance the quality and accessibility of care for the entire community.
Methods of Engaging and Supporting Local Communities
We employ various methods to engage and support the local communities. These include:
- Community Outreach Programs: Regular participation in health fairs, workshops, and educational events to raise awareness about health issues and provide resources to the community.
- Partnerships with Local Organizations: Collaborating with schools, community centers, and other organizations to offer health screenings, educational programs, and support services.
- Financial Support for Community Initiatives: Contributing financially to local health organizations and initiatives that promote community well-being.
- Mentorship Programs: Offering mentorship to aspiring healthcare professionals, fostering a legacy of care and support for the future of the community.
Technological Advancements
The past 60 years have witnessed a remarkable transformation in independent private practice, largely driven by technological advancements. These innovations have fundamentally altered how we interact with patients, manage appointments, and store crucial medical records. This evolution has not only improved efficiency but also enhanced the overall patient experience and the ability of practitioners to deliver superior care.Technological advancements have profoundly impacted independent private practice, streamlining processes and significantly enhancing patient care.
From rudimentary tools to sophisticated systems, technology has been a crucial partner in navigating the complexities of modern healthcare delivery.
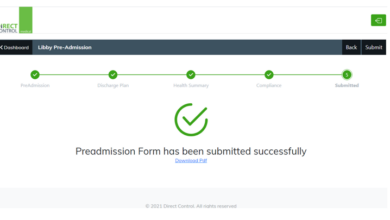
Evolution of Appointment Scheduling
The process of scheduling patient appointments has undergone a significant metamorphosis over the past six decades. Early methods relied heavily on paper calendars and phone calls, often leading to scheduling conflicts and administrative burdens. The introduction of computerized appointment scheduling systems dramatically improved efficiency. These systems allowed for more precise scheduling, reduced double-booking, and enabled patients to schedule appointments more conveniently through online portals.
Evolution of Record Keeping
The shift from paper-based medical records to electronic health records (EHRs) has revolutionized record keeping in independent private practice. Early systems relied on handwritten notes and physical files, which were often difficult to access and prone to errors. The advent of digital record keeping has facilitated easier access, improved accuracy, and streamlined the sharing of patient information.
Telehealth Integration
Telehealth has become an increasingly important component of independent private practice. Early iterations of telehealth, such as video consultations for follow-up appointments, have been invaluable for patients who live in remote areas or have mobility limitations. The rise of high-speed internet and advanced video conferencing technology has expanded the scope of telehealth services, allowing for remote diagnosis, treatment planning, and medication management.
Celebrating 60 years of providing independent private practice care, we’re excited to see the positive changes happening in our community. Oshkosh is experiencing exciting growth, with new development near the Fox River, like the project detailed in this article oshkosh eyes new development near fox river. This aligns perfectly with our commitment to fostering a thriving environment for our patients and the wider Oshkosh community, a commitment we’ve maintained for over six decades.
Comparison of Technological Advancements
Several technological advancements have significantly influenced independent private practice over the past 60 years. The transition from paper-based records to electronic health records (EHRs) has revolutionized patient data management, enabling easier access and improved accuracy. The implementation of telehealth platforms has expanded access to care, particularly for patients in remote locations. The development of appointment scheduling software has streamlined administrative tasks, reducing scheduling conflicts and improving patient convenience.
Impact on Patient Care and Communication
Technological advancements have significantly improved patient care and communication. Telehealth has enabled remote consultations, increasing accessibility for patients in various circumstances. Electronic health records (EHRs) have improved the accuracy and efficiency of patient data management, enabling clinicians to access and share patient information more easily. Communication tools, such as secure messaging systems, have facilitated faster and more efficient communication between patients and practitioners.
Table: Technological Advancements in Patient Scheduling and Record Keeping
| Technology | Year Introduced | Impact on Appointments | Impact on Records |
|---|---|---|---|
| Paper calendars and phone calls | Pre-1960s | Prone to scheduling conflicts, inefficient | Difficult to access, prone to errors |
| Computerized appointment scheduling systems | 1980s-1990s | Reduced double-booking, improved efficiency, easier scheduling for patients | Improved organization, easier retrieval of records |
| Electronic health records (EHRs) | 1990s-2000s | No direct impact on appointment scheduling, but improved coordination | Digital storage, enhanced accuracy, accessibility |
| Telehealth platforms | 2000s-present | Expanded appointment options, remote consultations possible | Data integration with EHRs, enabling remote monitoring |
| Secure messaging systems | 2000s-present | Faster communication, reduced wait times | Facilitated communication, improved record-keeping |
Future Trends
Looking ahead, the next 60 years promise both exciting opportunities and significant challenges for independent private practice. Adapting to evolving healthcare models, embracing technological advancements, and anticipating patient expectations are crucial for continued success. The landscape is dynamic, requiring a proactive and forward-thinking approach.The future of independent private practice hinges on a nuanced understanding of emerging trends and a willingness to adapt.
Independent practitioners must not only maintain high-quality care but also position themselves to thrive in an increasingly complex and competitive healthcare environment.
Potential Future Trends in Healthcare Models
Independent private practices will need to navigate the evolving healthcare landscape, which includes the rise of value-based care models. This shift emphasizes preventative care and patient outcomes over fee-for-service models. Practices that successfully integrate these principles into their operations will likely experience greater success. Other emerging models include patient-centered medical homes and accountable care organizations, where coordinated care across multiple providers becomes essential.
Impact of Emerging Healthcare Models on Independent Practices
Independent practices will need to strategically position themselves within these emerging healthcare models. This may involve collaborating with other providers, adopting new technologies, and focusing on preventative care and holistic patient well-being. Adapting to shared decision-making and team-based care approaches will be critical for success.
The Role of Technology in Shaping the Future of Independent Practice
Technology will undoubtedly play a pivotal role in shaping the future of independent practice. Telemedicine, electronic health records (EHRs), and patient portals will be increasingly important for remote consultations, efficient data management, and improved patient communication. The ability to leverage technology for enhanced efficiency and patient engagement will be key. Practices that fail to adapt will find themselves at a disadvantage.
Patient Expectations in the Next 60 Years
Patient expectations will likely evolve significantly in the next 60 years. Patients will likely expect more personalized, proactive, and convenient care. Accessibility, transparency, and a focus on patient experience will be crucial. A high level of trust and communication will be paramount. This necessitates a proactive approach to communication and relationship-building with patients.
Strategies for Adapting to Future Challenges and Opportunities
Several strategies can help independent practices adapt to future challenges and capitalize on opportunities. These include:
- Investing in technology: Implementing telehealth platforms, robust EHR systems, and patient portals will be essential to improve efficiency, communication, and access to care. This will allow practices to provide convenient and personalized services.
- Embracing value-based care: Transitioning from a fee-for-service model to a value-based care model will focus on preventative care, improved patient outcomes, and cost-effectiveness. This shift requires a proactive approach to population health management.
- Cultivating strong relationships: Building strong relationships with other healthcare providers and specialists will enable collaborative care and provide patients with comprehensive care. This also fosters trust and shared responsibility.
- Focusing on patient experience: Creating a positive and seamless patient experience will be crucial for attracting and retaining patients. This involves understanding and addressing patient needs, actively soliciting feedback, and promoting proactive communication.
Conclusion

In conclusion, 60 years of independent private practice care has witnessed remarkable evolution. The story, from historical significance to future trends, underscores the enduring commitment of independent practitioners to providing exceptional care. This journey has been influenced by societal changes, technological advancements, and evolving patient needs. Looking ahead, adapting to these forces will be critical for the continued success of independent practices.