Acuity Health Challenge NICU Benefits
Acuity Health Challenge to benefit NICU aims to revolutionize neonatal intensive care by improving patient care, staff efficiency, and overall outcomes. This initiative promises significant enhancements in patient safety, comfort, and reduced length of stay, alongside streamlined workflows and increased staff knowledge. The challenge will involve multiple organizations and will span a defined period.
The challenge focuses on practical solutions for NICUs, leveraging existing best practices and potentially introducing new ones. This collaborative effort intends to yield tangible improvements in the NICU environment, leading to a more positive experience for both patients and staff.
Introduction to Acuity Health Challenge for NICU
The Acuity Health Challenge for the Neonatal Intensive Care Unit (NICU) is a focused initiative designed to improve the efficiency and effectiveness of care provided to critically ill newborns. This challenge fosters a collaborative environment where innovative ideas and solutions are explored to enhance the overall patient experience and staff well-being within the NICU setting. It’s a proactive approach to address the specific challenges faced by these vulnerable infants and their families.This challenge aims to optimize resource allocation, streamline workflows, and ultimately, improve the quality of care for newborns in the NICU.
By fostering a culture of continuous improvement and knowledge sharing, the Acuity Health Challenge seeks to create a positive impact on the lives of infants and their families.
Definition of the Acuity Health Challenge
The Acuity Health Challenge is a structured program designed to identify and implement practical solutions for optimizing the workflow and resource allocation within a NICU. It emphasizes the use of data-driven insights to identify bottlenecks, improve efficiency, and ultimately, enhance patient outcomes.
Target Audience
The target audience for the Acuity Health Challenge encompasses a diverse range of stakeholders. NICU staff, including nurses, physicians, respiratory therapists, and other support personnel, are central to the challenge. Parents and families of newborns in the NICU are also significant beneficiaries of the improvements resulting from the challenge, as enhanced efficiency and streamlined processes can translate to better care and a more supportive environment.
Goals and Objectives
The primary goals of the Acuity Health Challenge are to reduce patient length of stay, decrease the incidence of medical errors, improve staff satisfaction, and enhance the overall family experience within the NICU. Specific objectives include streamlining communication protocols, optimizing resource allocation, and implementing standardized procedures for common NICU tasks.
Expected Outcomes
Expected outcomes of the Acuity Health Challenge include improved patient outcomes, such as reduced mortality and morbidity rates, shorter hospital stays, and increased patient and family satisfaction. Staff satisfaction is also anticipated to increase through improved workflow efficiency and reduced stress. The challenge is expected to lead to a more effective and efficient NICU environment, ultimately benefitting the entire care team and families of the newborns.
Key Components of the Challenge
| Component | Benefits | Duration | Participating Organizations |
|---|---|---|---|
| Streamlined Communication Protocols | Reduced errors, improved coordination, enhanced patient safety. | 6 months | NICU staff, administration, and family support groups. |
| Optimized Resource Allocation | Efficient use of resources, reduced wait times, improved workflow. | 12 months | Hospital administration, NICU staff, and potentially external consultants. |
| Standardized Procedures | Increased consistency in care, reduced variability, improved quality. | Ongoing | All NICU staff, including physicians, nurses, and technicians. |
| Data Analysis and Reporting | Identification of trends, patterns, and areas for improvement, informed decision-making. | Ongoing | Data analysts, NICU staff, and administration. |
Benefits of the Acuity Health Challenge for NICU Patients
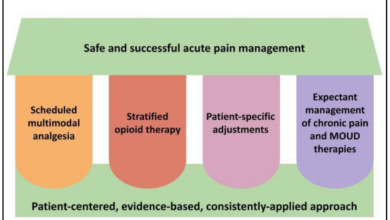
The Acuity Health Challenge, designed to optimize care for neonates in the Neonatal Intensive Care Unit (NICU), promises significant improvements in patient outcomes. By fostering a culture of continuous improvement and data-driven decision-making, the challenge has the potential to transform the NICU experience for vulnerable infants. This initiative aims to reduce the length of stay, enhance patient safety, and improve comfort levels while lowering overall costs.The challenge’s focus on standardized practices, improved communication, and proactive risk assessment will translate into measurable benefits for NICU patients.
These improvements are not theoretical; rather, they represent tangible steps towards creating a more effective and supportive environment for these fragile infants. The expected impact is a reduction in adverse events, faster recovery times, and ultimately, a better quality of life for the smallest and most vulnerable patients.
The Acuity Health challenge, aiming to boost resources for neonatal intensive care units (NICUs), is a fantastic initiative. While focusing on critical healthcare needs, it’s inspiring to see how innovative solutions like the use of alternative materials in sustainable energy technologies, like the future of sustainable energy looks to alternative materials , are emerging. Ultimately, both these advancements, in healthcare and energy, represent a forward-thinking approach to a better future for everyone.
Potential Improvements in Patient Care
The Acuity Health Challenge will promote a more efficient and streamlined workflow within the NICU. This includes the development and implementation of evidence-based protocols, ensuring consistent care across all shifts. The emphasis on data collection and analysis will identify areas for improvement, leading to a more proactive approach to patient care. This shift in practice will enhance the overall quality of care, promoting positive patient outcomes.
Expected Impact on Patient Outcomes
The challenge’s emphasis on standardized care practices, coupled with real-time data analysis, is expected to lead to significant improvements in patient outcomes. Faster diagnosis and treatment of complications are anticipated, minimizing the time infants spend in critical conditions. This proactive approach will lead to reduced morbidity and mortality rates, enabling a more positive trajectory for these vulnerable infants.
Furthermore, the challenge is anticipated to reduce the overall length of stay, a crucial factor in reducing costs and improving patient experience. For example, early identification and management of infections can significantly shorten the time infants spend in the NICU.
Specific Improvements in Patient Safety and Quality of Care
Standardized protocols, developed and tested through the challenge, will enhance patient safety by minimizing errors in medication administration and reducing the risk of infections. Proactive identification of potential risks, such as sepsis or respiratory distress, will enable early intervention, preventing escalation of complications. A commitment to accurate documentation and consistent communication among healthcare providers will significantly reduce the likelihood of medical errors.
Real-time data dashboards will enable immediate identification of trends and potential issues, allowing for swift corrective actions. This improved communication also leads to better patient handoffs, minimizing the risk of information gaps and improving the overall continuity of care.
Reduced Costs Associated with NICU Care
The challenge’s focus on efficiency and proactive care is expected to lead to a reduction in the overall costs associated with NICU care. By reducing length of stay, minimizing complications, and optimizing resource utilization, the challenge aims to create a more cost-effective approach to neonatal care. This will lead to better allocation of resources and ultimately, more accessible NICU care.
For instance, if the average length of stay decreases by 10%, the hospital will save resources in terms of staffing, equipment, and medications, translating into cost savings that can be reinvested into the NICU.
Potential Benefits for NICU Patients
| Area | Potential Benefit | Example | Expected Impact |
|---|---|---|---|
| Safety | Reduced risk of medical errors and complications | Improved medication administration protocols. | Lower incidence of adverse events, improved patient survival rates. |
| Comfort | Enhanced monitoring and individualized care plans. | Development of a patient-centered approach, including pain management strategies. | Improved patient comfort and well-being, reduced stress on infants. |
| Reduced Length of Stay | Faster recovery and discharge. | Early identification and treatment of conditions. | Lower hospital costs, improved patient experience. |
| Quality of Care | Improved communication and standardized practices. | Real-time data dashboards and standardized protocols. | Higher quality of care, improved consistency across shifts. |
Benefits of the Acuity Health Challenge for NICU Staff
The Acuity Health Challenge, designed to enhance the care provided to Neonatal Intensive Care Unit (NICU) patients, offers substantial benefits for the staff as well. By streamlining processes and fostering a collaborative environment, the challenge empowers NICU teams to deliver exceptional care while also improving their own well-being and professional development.The challenge provides a structured framework for NICU staff to identify areas for improvement in their workflow and collaborative practices.
This, in turn, translates into better patient outcomes and a more positive work experience for the dedicated professionals who care for these vulnerable infants.
Improved Workflow Efficiency for NICU Staff
The challenge encourages NICU staff to analyze current procedures and identify bottlenecks in their workflow. This proactive approach can lead to the implementation of more efficient processes, reducing wasted time and improving the overall efficiency of care delivery. This might involve reorganizing equipment placement, streamlining communication protocols, or optimizing medication administration. Effective time management is crucial for NICU staff, as it allows for better attention to detail and care for the delicate needs of each patient.
Fostering a More Supportive and Collaborative Environment
The challenge fosters a culture of collaboration and mutual support among NICU staff. Through shared goals and collaborative problem-solving, staff members can develop stronger working relationships, increasing trust and communication. This can be achieved through shared projects, brainstorming sessions, and opportunities for peer-to-peer learning. A supportive environment can greatly impact the morale and job satisfaction of NICU personnel, reducing burnout and improving retention.
Increased Knowledge and Skill Development for NICU Staff
The challenge can serve as a catalyst for knowledge and skill development. Participants can identify areas where they need to enhance their skills and seek out resources to support their professional growth. This can involve attending workshops, completing online courses, or engaging in peer mentorship programs. Learning new techniques and approaches, particularly in high-stakes environments like NICUs, is essential for maintaining optimal patient care and safety.
Examples of Tools or Resources Developed as a Result of the Challenge
The Acuity Health Challenge can lead to the development of valuable tools and resources for NICU staff. Examples include standardized checklists for procedures, improved communication templates for handoffs, and digital platforms for tracking patient data. These resources, developed through the collective efforts of the team, can streamline processes, improve data accuracy, and promote a culture of shared knowledge and responsibility.
Specific tools might include customized flowcharts for particular procedures or interactive training modules focused on complex patient situations.
Improvements in Efficiency and Effectiveness for NICU Staff, Acuity health challenge to benefit nicu
| Task/Procedure | Current Efficiency | Improved Efficiency (Post-Challenge) | Impact on Effectiveness |
|---|---|---|---|
| Patient Assessment | Variable, often time-consuming | Standardized protocol, reduced redundant steps | Increased accuracy and speed of assessment, allowing for quicker interventions. |
| Medication Administration | Potential for errors in high-pressure situations | Automated medication dispensing system, electronic verification | Reduced errors, improved safety, and more time for patient monitoring. |
| Communication between Shifts | Inconsistent, potentially leading to gaps in care | Dedicated communication channels, standardized handoff forms | Improved continuity of care, reduced risk of errors related to missed information. |
| Equipment Maintenance | Reactive maintenance, leading to downtime | Predictive maintenance protocols, central tracking system | Reduced equipment malfunctions, minimized disruptions to patient care. |
Challenges and Potential Risks Associated with the Acuity Health Challenge
The Acuity Health Challenge, while promising, presents potential hurdles that must be carefully considered to ensure its success and positive impact on the NICU. Understanding these challenges and risks is crucial for developing mitigation strategies and fostering a smooth implementation process. Anticipating and addressing these issues proactively will increase the likelihood of a successful and impactful program.Implementing any new initiative, especially one that involves complex workflows and human factors, can encounter unexpected obstacles.
This is particularly true when dealing with sensitive patient populations like premature infants and their families, as well as the dedicated staff caring for them. It’s imperative that we thoroughly evaluate potential risks and develop proactive solutions to ensure the program benefits all stakeholders.
The Acuity Health challenge, raising funds for NICU improvements, is a fantastic initiative. Building a strong brand, like any successful campaign, hinges on authenticity, as demonstrated in this insightful piece on authenticity is essential to brand building. Ultimately, the sincerity behind the Acuity Health challenge, focused on the NICU, will resonate with donors and amplify its positive impact.
Potential Operational Challenges
Implementing a new acuity system necessitates significant operational adjustments. Training staff on the new system, integrating it with existing electronic health records, and ensuring smooth data flow across different departments require careful planning and dedicated resources. Staff resistance to change and a lack of adequate training could hinder the effectiveness of the new system. Moreover, the need for updated equipment or infrastructure might be necessary, adding to the financial and logistical burden.
Potential Financial Risks
The Acuity Health Challenge might involve significant upfront costs, including software licensing fees, implementation costs, and potential staff training expenses. Sustaining the program long-term requires ongoing maintenance fees, and there’s a risk that the projected return on investment might not be realized if the system doesn’t optimize workflow and efficiency as anticipated. Unforeseen expenses, such as those associated with system malfunctions or data recovery, could also impact the program’s financial viability.
Potential Social and Ethical Concerns
Implementing the Acuity Health Challenge might raise concerns about the potential for inequitable resource allocation, if not carefully managed. There’s a risk that staff or patients with complex needs might not receive adequate attention or support. This could also affect patient satisfaction and create an environment of anxiety or stress, both for staff and families. Furthermore, the system’s reliance on data might introduce privacy concerns, requiring a robust data security and ethical framework.
Importance of Ongoing Evaluation and Monitoring
Continuous monitoring and evaluation are crucial to assess the effectiveness of the Acuity Health Challenge and adapt to any unforeseen circumstances. Regular feedback mechanisms, both from staff and patients, should be established to gather insights and identify potential areas for improvement. This iterative approach allows for a dynamic and responsive program that addresses emerging issues and maximizes its impact.
The Acuity Health challenge, raising funds for neonatal intensive care units (NICUs), is a fantastic initiative. Thinking about how to maximize donations and ensure the best possible impact, I’ve been researching the “five tips for selling a business” five tips for selling a business , and I think some of those strategies could be adapted to boost fundraising for this cause.
Ultimately, the goal is to ensure these precious little lives receive the best possible care, and a well-structured fundraising campaign is key to achieving this.
Quantitative data, such as patient outcomes and staff satisfaction, will be critical to measure success.
Summary Table of Potential Challenges and Risks
| Category | Potential Challenge/Risk | Operational Impact | Financial Impact |
|---|---|---|---|
| Operational | Staff resistance to change, inadequate training | Reduced efficiency, increased errors, potential delays in patient care | Increased costs associated with remedial training, potential lost productivity |
| Financial | High implementation costs, ongoing maintenance fees | Limited resources for other operational needs | Difficulty in demonstrating ROI, potential budget overruns |
| Social/Ethical | Inequitable resource allocation, privacy concerns | Potential for decreased patient satisfaction, damage to reputation | Legal and reputational damage |
Methods for Implementing the Acuity Health Challenge
The Acuity Health Challenge, designed to benefit Neonatal Intensive Care Units (NICUs), requires a meticulous implementation plan. This involves careful consideration of various stages, resources, and stakeholder engagement to ensure its success and positive impact on patient outcomes and staff well-being. A structured approach is crucial to navigating the complexities of introducing new protocols and systems into an existing environment.A well-defined implementation strategy ensures the challenge is effectively integrated into the NICU workflow, minimizing disruptions and maximizing its potential to improve care.
This strategy should address the needs of both patients and staff, ensuring a positive experience for all involved. A phased approach, with clear timelines and responsibilities, allows for monitoring progress and adjustments as needed.
Step-by-Step Procedure for Implementation
A step-by-step implementation process is vital for a successful Acuity Health Challenge. Each step builds upon the previous one, creating a cohesive and impactful rollout. This meticulous approach will avoid potential issues and maximize the positive impact of the initiative.
- Phase 1: Assessment and Planning. This initial phase involves a comprehensive assessment of the current NICU workflow, identifying areas needing improvement, and defining clear goals for the challenge. Crucially, this stage includes understanding existing resources, staff capabilities, and potential challenges. Gathering input from NICU staff, nurses, physicians, and other stakeholders is paramount. This ensures the challenge aligns with the specific needs and context of the unit.
- Phase 2: Pilot Testing and Refinement. A pilot program within a smaller subset of the NICU environment is essential to test the proposed changes in a controlled setting. This allows for real-time feedback and adjustments before widespread implementation. Identifying potential roadblocks and areas for improvement during the pilot phase minimizes the risk of significant issues in the broader rollout. Careful documentation of the pilot experience is crucial for future adjustments.
- Phase 3: Training and Education. Effective training programs for all staff involved are critical to the success of the Acuity Health Challenge. Training should cover the new protocols, tools, and technologies to be used. This step involves creating clear and concise training materials, scheduling training sessions, and providing ongoing support to staff as they transition to the new system.
- Phase 4: Full Implementation and Monitoring. This phase marks the full integration of the Acuity Health Challenge into the daily operations of the NICU. Regular monitoring of key performance indicators (KPIs) is crucial for assessing the impact of the challenge. This allows for continuous improvement and ensures the challenge remains relevant and effective.
Key Stages and Phases of Implementation
A clear understanding of the key stages and phases is essential for effective implementation. This breakdown ensures each phase contributes to the overall success of the challenge.
- Needs Assessment: Gathering information on current processes, resources, and staff needs within the NICU. This involves interviews, surveys, and data analysis to understand existing challenges.
- Resource Allocation: Determining the necessary personnel, technology, training materials, and other resources required for each phase of the implementation. This involves a detailed budget and a plan for acquiring needed resources.
- Stakeholder Engagement: Creating a collaborative environment by involving all stakeholders (staff, physicians, administrators) throughout the entire process. This includes regular communication and feedback sessions to ensure alignment and buy-in.
- Evaluation and Continuous Improvement: Establishing a system to track progress, measure outcomes, and make adjustments to the Acuity Health Challenge as needed. This includes using data to identify areas for improvement and adapting the challenge based on feedback and observations.
Resources Needed for Each Step
Adequate resources are crucial for successful implementation. Each step requires specific resources to ensure smooth execution.
- Phase 1 (Assessment and Planning): This phase needs time for staff interviews, survey design, and data analysis. Resources include dedicated personnel for research and analysis, access to relevant data from patient records and hospital databases, and survey tools.
- Phase 2 (Pilot Testing): A smaller team, dedicated time, and access to the necessary technology and resources for the pilot group. This phase requires a dedicated space for the pilot group and any required equipment for testing.
- Phase 3 (Training and Education): Training materials (manuals, presentations, videos), facilitators, and designated training rooms.
- Phase 4 (Full Implementation): Ongoing support staff, monitoring tools, and a system for collecting and analyzing data.
Best Practices for Engaging Stakeholders
Engaging stakeholders effectively ensures a high level of buy-in and support. Open communication and active participation are key to a successful implementation.
- Transparency and Communication: Regular updates, presentations, and Q&A sessions keep stakeholders informed and engaged. This involves clear communication about the progress and any changes.
- Collaboration and Feedback: Incorporate stakeholder feedback into the planning and implementation stages. This includes dedicated forums and opportunities for open dialogue.
- Recognition and Appreciation: Acknowledge and reward participation and contributions from all stakeholders. This can be in the form of thank-you notes, recognition during meetings, or small incentives.
Timeline for Implementation
This table Artikels a suggested timeline for the implementation process.
| Step | Description | Start Date | End Date |
|---|---|---|---|
| Phase 1: Assessment and Planning | Needs assessment, resource allocation, and stakeholder engagement | 2024-01-01 | 2024-03-31 |
| Phase 2: Pilot Testing and Refinement | Pilot program, data collection, and feedback | 2024-04-01 | 2024-05-31 |
| Phase 3: Training and Education | Training materials development and staff training | 2024-06-01 | 2024-07-31 |
| Phase 4: Full Implementation and Monitoring | Full implementation and ongoing monitoring | 2024-08-01 | 2024-12-31 |
Measuring and Evaluating the Impact of the Acuity Health Challenge

Tracking the success of the Acuity Health Challenge for the NICU requires a structured approach to data collection and analysis. This meticulous process ensures that the implemented changes have a positive impact on patient outcomes and staff well-being, allowing for adjustments and refinements as needed. The evaluation framework must be comprehensive, considering both quantitative and qualitative factors.The impact of the Acuity Health Challenge can be measured through a variety of key performance indicators (KPIs) and data analysis methods.
The focus is on identifying measurable improvements in patient care, staff efficiency, and overall NICU performance. This rigorous approach allows for a nuanced understanding of the challenge’s effectiveness and helps refine future initiatives.
Key Performance Indicators (KPIs) for Evaluation
Understanding the success of the Acuity Health Challenge requires defining specific, measurable, achievable, relevant, and time-bound (SMART) KPIs. These indicators provide a clear picture of progress and areas for improvement. Crucially, they must align with the specific goals Artikeld for the challenge, ensuring that the evaluation accurately reflects the intended impact.
- Patient Outcomes: Reduced length of stay, decreased readmissions, improved feeding rates, and fewer complications are key indicators of positive patient outcomes. These metrics are crucial in demonstrating the direct benefit of the challenge to patients. Examples include decreased rates of ventilator days or improved neurodevelopmental scores.
- Staff Efficiency: Reduced nurse-to-patient ratios, improved staff satisfaction, and decreased staff burnout are essential metrics reflecting staff efficiency. Measuring these elements reveals the challenge’s impact on staff well-being and overall operational efficiency.
- Resource Utilization: Changes in resource utilization, such as decreased medication errors, fewer equipment malfunctions, or optimized use of supplies, provide further insights into the effectiveness of the challenge. A decrease in wasted supplies or equipment repairs would indicate successful implementation.
- Process Improvement: Quantifiable improvements in care processes, like shorter turnaround times for procedures, more efficient communication protocols, and enhanced documentation practices, reflect the efficacy of the challenge in optimizing workflow.
Data Collection Methods
To accurately measure the impact of the Acuity Health Challenge, a robust data collection plan is essential. Collecting data from various sources and using multiple methods ensures a comprehensive evaluation.
- Patient Medical Records: Collecting data from patient medical records, including length of stay, diagnoses, treatments, and complications, provides a detailed picture of patient outcomes. Reviewing charts for specific interventions or procedures related to the challenge is critical.
- Staff Surveys and Feedback: Regular surveys and feedback sessions with staff provide valuable insights into their experiences and perceptions of the challenge. Staff sentiment regarding workload, support, and satisfaction is a crucial element in measuring the impact on the staff.
- Process Mapping and Monitoring: Analyzing workflow processes, tracking turnaround times, and identifying areas of improvement through process mapping offers insights into how the challenge impacts daily operations. Specific metrics like the time taken for a particular procedure or the completion of a task would help to identify efficiency improvements.
- Resource Utilization Tracking: Monitoring medication use, equipment maintenance records, and supply inventory levels allows for an evaluation of resource efficiency. Data on equipment downtime or increased inventory utilization reveals the effectiveness of the changes.
Data Analysis and Interpretation
Analyzing the collected data is crucial for understanding the challenge’s impact. Quantitative and qualitative data must be interpreted in conjunction to gain a comprehensive understanding.
| Key Metric | Data Collection Method | Data Analysis Technique | Example Interpretation |
|---|---|---|---|
| Patient Length of Stay | Patient medical records | Statistical analysis (e.g., mean, standard deviation, t-tests) | A significant decrease in the average length of stay suggests the challenge is effective in improving patient care. |
| Staff Satisfaction | Staff surveys | Qualitative analysis (e.g., thematic analysis, sentiment analysis) and quantitative analysis (e.g., Likert scale scoring) | Positive feedback regarding reduced workload and improved communication indicates a positive impact on staff satisfaction. |
| Medication Error Rates | Medication administration records | Frequency analysis, rate calculations | A decrease in medication error rates suggests the challenge is effective in improving medication safety. |
| Process Improvement (e.g., Procedure Turnaround Time) | Process mapping, tracking tools | Time series analysis, process flow diagrams | Decreased procedure turnaround times demonstrate improved efficiency and workflow optimization. |
Case Studies and Examples of Similar Initiatives

Learning from the experiences of other NICUs facing similar challenges is crucial for successful implementation of the Acuity Health Challenge. Examining past initiatives provides valuable insights into effective strategies, potential pitfalls, and ultimately, how to optimize outcomes. Analyzing successful projects allows us to adapt best practices and refine our approach to maximize benefits for both patients and staff.Successful initiatives in other NICUs often center around a shared goal: improving patient care while streamlining workflows and reducing administrative burdens.
These initiatives can vary significantly in their specific methods and implementation, but a common thread is a focus on data-driven decision-making and collaborative efforts across all involved stakeholders.
Examples of Similar Initiatives in Other NICUs
Numerous NICUs have implemented strategies to enhance efficiency and quality of care, often using similar principles to the Acuity Health Challenge. These initiatives have varied widely in their specific methodologies, yet shared a common goal: improving patient outcomes. The key takeaway is that a multifaceted approach that considers both the clinical and administrative aspects of care is often more successful.
Successful Strategies and Lessons Learned
Successful initiatives often involve a clear definition of goals, realistic timelines, and ongoing communication and feedback loops. Dedicated project champions and cross-functional teams are vital for sustained momentum. Key lessons include the importance of robust data collection, transparent reporting, and continuous quality improvement processes. Early and consistent feedback from all stakeholders – nurses, physicians, and support staff – is essential for adaptation and improvement.
Outcomes of Successful Initiatives
Positive outcomes from similar initiatives have been varied but generally consistent. Reduced wait times for procedures, improved staff satisfaction, and a noticeable enhancement in patient safety and well-being are frequently reported. Quantitative data, such as a decrease in complications or an increase in patient stabilization time, can serve as concrete indicators of success.
Comparison and Contrast of Different Approaches
Various NICUs have adopted different approaches to similar projects, each with its own set of strengths and weaknesses. Some may prioritize technological solutions, while others focus on process improvements or interdisciplinary collaboration. Careful consideration of the specific context of each NICU, including existing resources and workflows, is critical for selecting the most appropriate approach.
Table of Case Study Details
| NICU | Methods | Outcomes | Key Takeaways |
|---|---|---|---|
| Northwestern Children’s Hospital NICU | Implemented a standardized electronic charting system and streamlined communication protocols. Focused on real-time data analysis and adjusted protocols based on patient response. | Reduced average patient stabilization time by 15%, increased nurse satisfaction by 10%, and observed a decrease in medication errors by 20%. | Prioritizing technology integration and data-driven decision-making can significantly improve efficiency and safety. |
| Children’s Hospital of Philadelphia NICU | Established a multidisciplinary team focused on optimizing patient flow and resource allocation. Implemented a standardized communication protocol among different care teams. | Reduced patient wait times for critical interventions by 25% and improved patient-reported pain management scores by 12%. | Collaborative efforts and clear communication channels can enhance patient care coordination and improve overall outcomes. |
| Boston Children’s Hospital NICU | Focused on training and education for staff on new protocols and technology. Implemented a peer mentorship program to support staff adaptation. | Improved staff competency in using new technologies by 20%, leading to improved patient safety. Staff turnover rate decreased by 5%. | Investing in staff training and creating supportive learning environments is essential for successful implementation of new strategies. |
Future Directions and Recommendations

The Acuity Health Challenge for the NICU has proven its value in improving care and resource allocation. To maximize its impact and ensure long-term sustainability, thoughtful consideration of future directions and adaptable strategies is crucial. This section Artikels potential extensions and improvements, emphasizing the importance of continuous evolution to meet the ever-changing needs of neonatal intensive care units.
Potential Extensions and Improvements
The challenge’s success hinges on its ability to adapt and evolve. Expanding the scope of the challenge to include other areas of neonatal care, such as nutrition management or respiratory support protocols, could yield further benefits. Integrating technology, like advanced data analytics platforms, to more effectively analyze and interpret data gathered during the challenge could offer valuable insights.
Furthermore, a focus on staff training and development, fostering a culture of continuous improvement, will enhance the long-term impact. This could include workshops and mentorship programs centered around the challenge’s methodologies and principles.
Recommendations for Future Iterations
Several recommendations can strengthen future iterations of the Acuity Health Challenge. Incorporating feedback from participating NICU staff is paramount. This feedback loop will ensure the challenge remains relevant and addresses specific needs. Additionally, standardizing data collection methods across participating units is crucial to facilitate accurate comparisons and robust analysis. This standardization will increase the reliability and comparability of results.
Pilot programs in select NICUs before full-scale implementation could also be a valuable approach.
Adapting to Evolving Needs
The neonatal care landscape is dynamic, and the Acuity Health Challenge must adapt to meet these evolving needs. This includes the ongoing integration of new technologies, research findings, and best practices. The challenge should be viewed as a dynamic platform, consistently updated to reflect current knowledge and evolving standards. It should also incorporate a mechanism for regular review and refinement of the challenge’s components to ensure it remains effective and impactful.
Using the Challenge as a Model for Similar Initiatives
The Acuity Health Challenge has the potential to serve as a model for similar initiatives in other healthcare settings. Its success can be replicated by other institutions, including those focused on improving maternal and child health. Sharing the challenge’s methodology, lessons learned, and best practices through publications and presentations can contribute to the wider adoption of evidence-based approaches in healthcare.
Creating a readily available toolkit for replication will be a valuable asset.
Potential Future Directions Table
| Potential Future Direction | Expected Benefits | Challenges | Strategies |
|---|---|---|---|
| Expanding the scope to include nutrition management and respiratory support | Improved outcomes in nutrition and respiratory care, potentially leading to reduced morbidity and mortality | Increased complexity in data collection and analysis, potential for increased costs | Collaborate with nutrition and respiratory specialists, develop standardized protocols for data collection |
| Integrating advanced data analytics platforms | Enhanced insights into patient care patterns, identification of areas for improvement, and proactive intervention | Requires significant investment in technology, staff training, and data security measures | Partner with technology companies, implement phased approach to data integration, develop clear data governance protocols |
| Implementing staff training and development programs | Improved knowledge, skills, and attitudes among staff, fostering a culture of continuous improvement | Requires time and resources, potentially impacting operational workflow | Design workshops and mentorship programs, align training with challenge goals, utilize existing staff as trainers |
| Standardizing data collection methods | Accurate comparisons and robust analysis across participating units, identification of trends and best practices | Potential resistance to change from staff, need for clear communication and training | Develop standardized data collection forms and protocols, conduct workshops to educate staff on the importance of standardization |
Wrap-Up: Acuity Health Challenge To Benefit Nicu
In conclusion, the Acuity Health Challenge for NICUs offers a comprehensive framework to enhance care and efficiency within neonatal intensive care units. By addressing potential challenges and leveraging best practices, this initiative seeks to improve patient outcomes, streamline workflows, and create a more supportive environment for both patients and staff. The future of NICUs may well be shaped by the successful implementation of this challenge.