Northeast Wisconsins Healthcare Future
The future of medical care in northeast Wisconsin is poised for exciting transformations. Challenges like access to specialists and affordability are intertwined with the opportunities presented by telehealth, AI, and evolving patient preferences. This exploration delves into the complexities, providing insights into the changes shaping healthcare in the region.
Current access to care varies across counties, with rural areas facing particular challenges. The projected shift in the healthcare workforce will demand innovative solutions. Technological advancements offer exciting possibilities for improved diagnostics, treatments, and accessibility, while the rising costs of care necessitate strategic planning.
Access to Care
Northeast Wisconsin’s healthcare landscape presents a complex picture of access and disparity. While the region boasts some excellent facilities, significant challenges persist, particularly in rural areas. Limited availability of specialists, coupled with a growing aging population, necessitates proactive strategies to ensure equitable access to quality care.Current access to medical care in Northeast Wisconsin faces challenges stemming from a combination of factors.
The future of medical care in Northeast Wisconsin looks promising, but access and affordability remain key concerns. Local initiatives, like sustaining our waters the fox wolf watershed alliance , show how community-based solutions can improve overall health and well-being, which ultimately supports the long-term health of our healthcare system. This interconnectedness highlights the need for comprehensive strategies to ensure the future of medical care in the region.
Rural communities often have fewer healthcare providers, leading to longer wait times for appointments, particularly with specialists. This disparity in access can exacerbate existing health inequities, impacting those with lower socioeconomic status or limited transportation options. Further complicating the situation is the projected decline in healthcare professionals in the region, demanding innovative solutions to mitigate these issues.
Projected Healthcare Workforce Changes
The healthcare workforce in Northeast Wisconsin is projected to experience a significant shift over the next decade. Factors like retirement of experienced professionals and the slower rate of new entrants into the field suggest a potential shortage of physicians, nurses, and other essential healthcare personnel. This trend mirrors national patterns, emphasizing the urgent need for proactive recruitment and retention strategies to address the anticipated shortfall.
For instance, the increasing complexity of medical treatments and procedures necessitates a larger pool of specialists and sub-specialists, but the anticipated workforce decline presents a significant obstacle.
Solutions for Improved Access
Several strategies can improve access to specialists and primary care providers in rural areas. Implementing telehealth programs can bridge geographical gaps, allowing patients in remote communities to connect with specialists. Collaborative care models, where primary care physicians work alongside specialists, can optimize resource allocation and reduce wait times for specialized care. Incentivizing medical professionals to practice in underserved areas through loan repayment programs or other financial incentives could also attract more providers to the region.
Furthermore, investing in training programs to develop a pipeline of local healthcare professionals is crucial for long-term sustainability.
Comparison of Healthcare Facilities
| County | Hospital Locations | Services Offered |
|---|---|---|
| Brown | [List of Hospitals and Clinics in Brown County] | [List of Services Offered in Brown County Hospitals] e.g., General Surgery, Cardiology, Oncology |
| Calumet | [List of Hospitals and Clinics in Calumet County] | [List of Services Offered in Calumet County Hospitals] e.g., Internal Medicine, Pediatrics, Emergency Care |
| Door | [List of Hospitals and Clinics in Door County] | [List of Services Offered in Door County Hospitals] e.g., Family Medicine, OB/GYN, Mental Health Services |
| Kewaunee | [List of Hospitals and Clinics in Kewaunee County] | [List of Services Offered in Kewaunee County Hospitals] e.g., Primary Care, Surgical Procedures, Diagnostics |
| Outagamie | [List of Hospitals and Clinics in Outagamie County] | [List of Services Offered in Outagamie County Hospitals] e.g., Orthopedics, Neuro-Surgery, Trauma Care |
| Sheboygan | [List of Hospitals and Clinics in Sheboygan County] | [List of Services Offered in Sheboygan County Hospitals] e.g., Neurosciences, Cardiac Care, Urgent Care |
| Winnebago | [List of Hospitals and Clinics in Winnebago County] | [List of Services Offered in Winnebago County Hospitals] e.g., Cardiovascular Services, Rehabilitation Services, and more |
This table provides a high-level overview of healthcare facilities and services in Northeast Wisconsin counties. Each county’s healthcare infrastructure and service offerings vary, highlighting the need for a nuanced approach to addressing access disparities across the region.
Technological Advancements
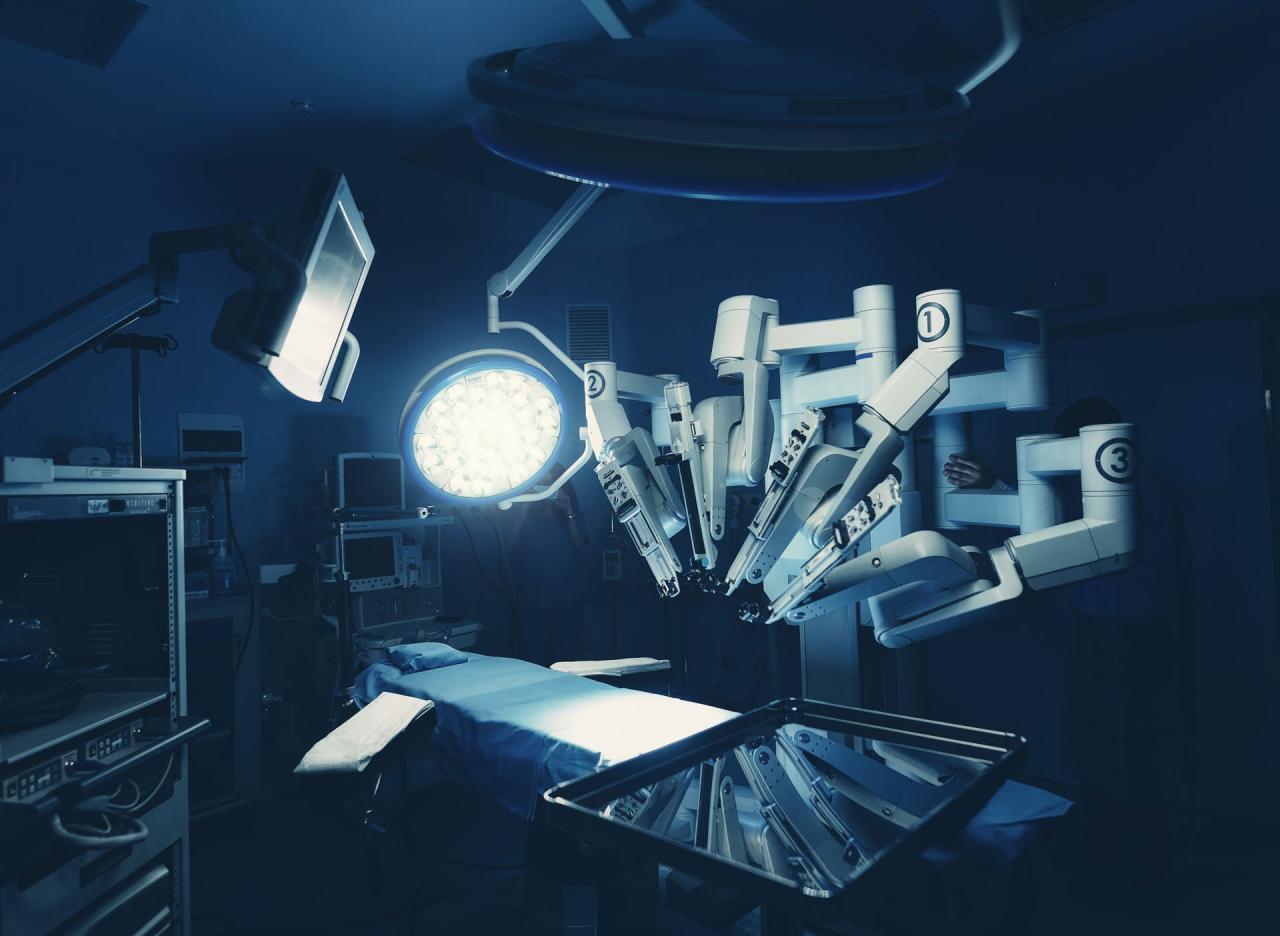
Northeast Wisconsin’s healthcare future hinges on embracing innovative technologies. Telehealth and remote patient monitoring are poised to revolutionize access and quality of care, particularly in rural areas. Artificial intelligence and machine learning hold significant promise for enhancing diagnostics and treatment strategies, while emerging technologies are likely to reshape the very fabric of medical practice. These advancements can lead to more efficient, personalized, and accessible healthcare, ultimately benefiting the entire community.The adoption of these technologies requires careful planning and consideration of the needs of diverse patient populations.
Addressing potential barriers, such as digital literacy and affordability, will be crucial to ensure equitable access to these advancements. By strategically integrating these technologies, Northeast Wisconsin can move toward a future of more effective, personalized, and accessible healthcare.
Telehealth and Remote Patient Monitoring
Telehealth and remote patient monitoring (RPM) are transforming healthcare delivery, enabling remote consultations, monitoring of vital signs, and medication management. These tools can extend access to specialists, particularly for those in underserved areas. Telehealth can also reduce travel time and costs for patients, improving convenience and adherence to treatment plans. RPM systems, by continuously tracking patients’ health data, can facilitate early detection of potential issues and prompt intervention, potentially preventing hospitalizations and improving patient outcomes.
Artificial Intelligence and Machine Learning in Healthcare
Artificial intelligence (AI) and machine learning (ML) are increasingly impacting diagnostics and treatment plans. AI algorithms can analyze medical images (X-rays, CT scans, MRIs) with remarkable accuracy, assisting radiologists in detecting anomalies. Furthermore, AI can analyze patient data to predict potential health risks, identify optimal treatment pathways, and personalize medication regimens. This personalized approach can significantly improve patient outcomes and reduce healthcare costs.
For instance, AI-powered diagnostic tools are already being used to detect skin cancer with greater accuracy than traditional methods. Machine learning can also predict the likelihood of readmission in hospitals.
Emerging Technologies
Several emerging technologies are poised to revolutionize medical care. 3D printing is transforming surgical planning and prosthetics, enabling the creation of highly customized and personalized solutions. Virtual reality (VR) and augmented reality (VR) are being explored for pain management, rehabilitation, and surgical training. Wearable sensors and bio-integrated devices can continuously monitor patients’ health, providing real-time data for proactive interventions and personalized care.
These advancements, along with the integration of big data analytics, can offer a wealth of information to healthcare providers for better decision-making.
Telehealth Platform Comparison
| Telehealth Platform | Advantages | Disadvantages | Suitable Patient Populations |
|---|---|---|---|
| Video conferencing platforms (e.g., Zoom, Google Meet) | Ease of use, readily available, often free/low-cost options | Potential for technical difficulties, less secure than dedicated platforms, limited features for complex patient care | Patients needing basic consultations, follow-up appointments, and those comfortable with technology |
| Dedicated telehealth platforms (e.g., Teladoc, Amwell) | Enhanced security, advanced features (e.g., secure messaging, remote monitoring), dedicated support | Higher costs, potentially less user-friendly for patients unfamiliar with the platform | Patients requiring complex monitoring, those needing access to specialists, or those requiring secure communication |
| Mobile apps | Accessibility through smartphones, convenience for remote monitoring | Potential data security concerns, limited functionality compared to dedicated platforms, may require specific devices or software | Patients comfortable with mobile technology, those needing simple health data tracking and basic consultations |
Cost of Care
Northeast Wisconsin’s healthcare landscape is facing the same pressures as the rest of the nation, with rising costs posing a significant challenge to both patients and providers. Understanding these costs and potential solutions is crucial for ensuring access to quality care for all residents. The rising price of everything, from pharmaceuticals to hospital stays, is impacting the affordability of medical services.The current cost of medical care in Northeast Wisconsin is likely higher than the national average for certain services, particularly specialized care and treatments.
Factors like the region’s demographics, the availability of providers, and the cost of living contribute to this difference. Access to specialized care might be more expensive due to the limited number of providers and higher overhead costs associated with maintaining specialized equipment and training. The same can be said for certain rural areas.
Current Cost Analysis
The current cost of medical care in Northeast Wisconsin is affected by factors such as insurance coverage, provider availability, and local economic conditions. Comparing Northeast Wisconsin’s costs to national averages requires careful consideration of these local factors.
Future Healthcare Cost Projections
Future healthcare costs in Northeast Wisconsin are anticipated to rise due to inflation and population growth. Population growth, particularly among the elderly, often increases the demand for healthcare services. Inflation affects the cost of everything, from medical supplies to personnel. Healthcare inflation is often higher than the general inflation rate.
Strategies for Cost Control
Controlling healthcare costs requires a multi-faceted approach. Improving preventative care can reduce the need for costly treatments in the future. Negotiating better rates with providers and insurance companies is another crucial strategy. Promoting the use of telehealth can reduce the costs associated with in-person visits, especially for routine checkups and follow-ups.
Projected Healthcare Spending Trends
| Healthcare Service | Projected Spending (2024-2028) | Projected Spending (2029-2033) |
|---|---|---|
| Primary Care | $5,000 – $6,000 per patient per year | $5,500 – $7,000 per patient per year |
| Specialty Care | $10,000 – $15,000 per patient per year | $12,000 – $18,000 per patient per year |
| Hospitalizations | $20,000 – $30,000 per admission | $25,000 – $40,000 per admission |
| Prescription Drugs | $1,000 – $2,000 per patient per year | $1,200 – $2,500 per patient per year |
The table above provides a simplified projection. Actual costs may vary based on individual circumstances, specific treatments, and the availability of cost-effective care.
Community Health
Northeast Wisconsin’s vibrant communities face unique health challenges intertwined with socioeconomic factors. Understanding these factors and implementing proactive strategies is crucial for fostering a healthier population. This involves addressing the root causes of disparities and empowering communities to take control of their well-being. This section explores strategies for promoting community health initiatives to improve overall well-being, highlighting the vital role of community health workers.Socioeconomic factors significantly impact health outcomes in Northeast Wisconsin.
Poverty, limited access to nutritious food, inadequate housing, and lack of transportation can all contribute to higher rates of chronic diseases, mental health issues, and lower life expectancy. For example, areas with higher unemployment rates often show a correlation with increased rates of diabetes and cardiovascular disease due to stress and limited access to healthy food options. Addressing these underlying issues is essential for creating a healthier and more equitable community.
The future of medical care in Northeast Wisconsin is looking promising, with new clinics and hospitals popping up. However, as we consider the region’s growing needs, it’s important to think about sustainable practices. Just like the future of sustainable energy looks to alternative materials, like those explored in this article ( the future of sustainable energy looks to alternative materials ), we need to explore sustainable solutions for healthcare in the region, from energy use to waste management.
This will ensure a healthy and thriving future for everyone in Northeast Wisconsin.
Impact of Socioeconomic Factors on Health Outcomes
Northeast Wisconsin, like many regions, experiences disparities in health outcomes tied to socioeconomic factors. Lower income often correlates with limited access to quality healthcare, healthy food options, and safe housing. These conditions can exacerbate existing health issues and create barriers to preventative care. For instance, limited access to transportation can hinder individuals from attending regular check-ups or accessing vital community resources.
Moreover, the stress associated with financial insecurity and unstable housing can negatively impact mental health and overall well-being.
Strategies for Promoting Community Health Initiatives
Promoting community health initiatives requires a multifaceted approach that engages community members, leverages resources, and addresses the root causes of health disparities. Collaboration between healthcare providers, community organizations, and local governments is essential. One successful strategy is the implementation of community gardens and mobile farmers’ markets to increase access to fresh produce in low-income neighborhoods. Additionally, educational programs focusing on healthy eating habits, stress management techniques, and the importance of regular check-ups can empower individuals to take control of their health.
Role of Community Health Workers
Community health workers (CHWs) play a critical role in providing preventative care and support within communities. They act as trusted intermediaries between the healthcare system and community members, fostering trust and facilitating access to essential services. Their role extends beyond basic health education; they often provide emotional support, navigate complex systems, and empower individuals to make informed health decisions.
For instance, a CHW might assist a family in accessing food banks, connecting them with resources for childcare, and providing encouragement for adopting healthier lifestyles.
Community Health Programs and Initiatives in Northeast Wisconsin
| Program Name | Description | Target Population |
|---|---|---|
| Northeast Wisconsin Community Health Coalition | A collaborative network of organizations working to improve health outcomes in the region. | Diverse community members, particularly those with limited access to care. |
| Healthy Start Coalition | Focuses on improving the health and well-being of pregnant women and young children. | Pregnant women, infants, and toddlers. |
| Local Food Bank Partnerships | Collaborations with food banks to increase access to nutritious food for those in need. | Low-income individuals and families. |
| Mental Health Awareness Programs | Educational workshops and support groups to raise awareness and reduce stigma associated with mental health conditions. | Individuals and families experiencing mental health challenges. |
Public Health Infrastructure
Northeast Wisconsin’s public health infrastructure plays a crucial role in maintaining the well-being of its residents. However, the region faces challenges in effectively addressing emerging health concerns and ensuring equitable access to preventative services. This discussion examines the current state of public health infrastructure, the importance of preventative measures, and strategies for optimizing resources and strengthening preparedness.The current state of public health infrastructure in Northeast Wisconsin is characterized by a mix of strengths and weaknesses.
Local health departments often operate with limited resources, which can impact their ability to implement comprehensive programs and respond to outbreaks. This is a common issue in rural areas, often requiring greater collaboration and shared resources with neighboring communities or state agencies to achieve adequate coverage.
Current Public Health Capacity
The public health infrastructure in Northeast Wisconsin comprises local health departments, community organizations, and partnerships with state agencies. These entities are often tasked with providing essential services like disease surveillance, immunizations, and chronic disease management. However, resource limitations can impede the ability to provide comprehensive services across the entire region, especially in areas with sparse populations.
Importance of Preventative Measures
Preventative measures are crucial in reducing the burden of chronic diseases, a significant health concern in the region. Promoting healthy lifestyles, including proper nutrition, regular exercise, and smoking cessation, can significantly decrease the risk of developing conditions like heart disease, diabetes, and certain cancers. The implementation of public health initiatives that encourage these behaviors is vital for long-term health improvements.
Optimizing Public Health Resources
Optimizing public health resources involves strategic planning and collaboration. This includes enhancing data collection and analysis to identify emerging health trends and disparities. By leveraging technology and implementing community-based interventions, resources can be allocated more effectively. Collaboration between local health departments, community organizations, and healthcare providers is key to addressing complex health issues. For instance, the implementation of telehealth platforms could expand access to preventative care in remote areas.
Strengthening Public Health Preparedness and Response
Strengthening public health preparedness and response requires a multi-faceted approach. This includes developing and regularly updating emergency response plans to effectively address potential outbreaks or health crises. Training and equipping public health personnel with the necessary skills and resources is vital for swift and efficient responses. Investing in infrastructure for rapid disease surveillance and diagnostics is also crucial.
The future of medical care in northeast Wisconsin is looking pretty interesting. With Oshkosh eyes on new development near the Fox River, like the recent project oshkosh eyes new development near fox river , it suggests a potential boost in the area’s economic vitality. This could lead to more investment in healthcare facilities and better access to specialized care for the region’s residents, ultimately improving the future of medical care in the area.
A good example is the proactive implementation of public health measures during the COVID-19 pandemic. The lessons learned from this event can inform future preparedness strategies. Regular community engagement and education are vital to building public trust and facilitating cooperation in emergency situations. For example, clear communication strategies and community awareness campaigns can be used to promote preparedness.
Rural Healthcare Models

Northeast Wisconsin, like many rural communities, faces unique challenges in providing accessible and high-quality healthcare. The geographical dispersion of the population, coupled with a shortage of healthcare professionals, often leads to longer travel times for patients and limited specialist options. This necessitates innovative solutions and tailored healthcare models to address these specific needs. Finding the right balance between affordability, accessibility, and quality is paramount.Rural healthcare models need to be adaptable and responsive to the unique needs of the community.
This requires a focus on integrated care, telehealth solutions, and community partnerships to overcome the challenges of isolation and limited resources.
Comparing Rural Healthcare Models
Different models for rural healthcare delivery cater to specific strengths and weaknesses of a community. A key distinction lies between traditional models that rely heavily on centralized facilities and newer models that emphasize decentralized care and community engagement. Traditional models often struggle with access and the cost of maintaining facilities, while newer models can be more efficient in utilizing resources and addressing the unique needs of rural communities.
Best Practices for Integrated Care
Implementing integrated care models in rural settings requires a multi-faceted approach. First, establishing strong collaborations between primary care providers, specialists, and community health workers is crucial. This allows for a more holistic view of patient care and ensures seamless transitions between different levels of care. Second, leveraging technology like telehealth can bridge geographical gaps, allowing patients to access specialists and receive ongoing care without extensive travel.
Finally, actively engaging local communities and incorporating their input into the design and implementation of care models is essential for long-term sustainability and success.
Innovative Solutions for Addressing Healthcare Challenges
Several innovative solutions can address healthcare challenges specific to rural communities. One example is the use of mobile health units, which can bring essential services directly to underserved areas, thereby reducing travel times and improving access. Furthermore, the establishment of community health centers, equipped with a range of services, can improve access to care and reduce the burden on already stretched resources.
Table of Rural Healthcare Models, The future of medical care in northeast wisconsin
| Healthcare Model | Key Characteristics | Applicability to Northeast Wisconsin |
|---|---|---|
| Community Health Centers | Offer a wide range of services in one location, including primary care, dental, mental health, and substance abuse treatment. | High. Addresses the need for comprehensive care in smaller towns and rural areas. |
| Federated Models | Multiple providers and facilities collaborate to share resources and provide a broader range of services. | Medium-High. Requires strong leadership and cooperation between different healthcare organizations. |
| Rural Health Clinics | Offer primary care services in underserved areas, often with nurse practitioners and physician assistants. | High. Effectively addresses the shortage of physicians in rural areas. |
| Telehealth Platforms | Provide remote access to specialists and other healthcare services. | High. Can overcome geographical barriers and increase access to specialists. |
| Mobile Health Units | Bring healthcare services directly to rural communities through mobile clinics. | Medium-High. Especially beneficial for populations in remote areas or those with limited transportation options. |
Patient Preferences
Northeast Wisconsin’s healthcare future hinges on understanding and responding to patient preferences. The evolving needs and expectations of patients will significantly shape the design and delivery of medical services in the region. This section explores key patient preferences, anticipated changes, and strategies to ensure future healthcare models align with these priorities.Patient expectations are not static; they are dynamic, influenced by societal shifts, technological advancements, and personal experiences.
The desire for personalized care, convenience, and a seamless patient journey is likely to increase. Understanding how these expectations translate into concrete needs is crucial for tailoring services effectively.
Patient Preferences Regarding Healthcare Delivery
Patients in Northeast Wisconsin, like elsewhere, value accessibility, convenience, and quality of care. Factors influencing these preferences include proximity to facilities, wait times, and the availability of various service options. Furthermore, patients increasingly seek options that integrate technology, allowing them to manage their health proactively and participate more actively in their care. This includes telehealth consultations, online appointment scheduling, and access to personalized health records.
Evolving Patient Needs and Expectations
The demand for personalized medicine is rising. Patients desire treatment plans tailored to their individual needs and preferences. This trend is being driven by the increasing availability of genetic information and the growing understanding of individual biological variations. Similarly, patients are becoming more health-conscious and are seeking proactive health management tools. This includes preventative care options, access to health information, and resources for self-care.
Strategies for Aligning Future Healthcare Models with Patient Priorities
A key strategy for future healthcare models is to incorporate patient feedback into the planning process. This involves active listening to patients’ concerns, incorporating their input into service design, and proactively seeking their feedback through surveys, focus groups, and direct interaction. Utilizing technology to gather and analyze patient feedback can create a more responsive and efficient process.
Incorporating Patient Feedback into Healthcare Planning
Gathering and analyzing patient feedback is critical for healthcare planning. This involves establishing mechanisms for collecting data through various channels. For example, patient satisfaction surveys, online feedback forms, and focus groups can provide valuable insights. Additionally, active listening during patient interactions and analyzing data on utilization patterns can be invaluable. Utilizing this feedback ensures that the healthcare system adapts to evolving patient needs and priorities.
Data collected through various channels should be analyzed to identify common themes and areas for improvement.
Closing Summary: The Future Of Medical Care In Northeast Wisconsin
Northeast Wisconsin’s healthcare future is a tapestry woven from the threads of access, technology, cost, community well-being, and patient preferences. Addressing the unique challenges of rural communities, while embracing technological advancements and community-focused initiatives, will be crucial in shaping a future of accessible, affordable, and high-quality care. Ultimately, the goal is to create a robust and resilient healthcare system that caters to the evolving needs of the region’s diverse population.