Northeast Wisconsins Health Transformation
Transforming northeast wisconsins health through direct primary care – Transforming Northeast Wisconsin’s health through direct primary care sets the stage for a vital conversation about improving access and affordability. This initiative explores the potential of direct primary care (DPC) models to address the unique healthcare needs of the region, considering both benefits and challenges. The evolving healthcare landscape demands innovative solutions, and DPC presents a compelling opportunity for change.
This in-depth look at the potential impact of DPC in Northeast Wisconsin delves into the current healthcare landscape, examining specific population needs, access disparities, and existing barriers. The discussion encompasses strategies for community engagement, sustainable models, workforce requirements, and potential pitfalls. Illustrative case studies and a comprehensive analysis of potential challenges provide a nuanced perspective on this crucial issue.
Introduction to Direct Primary Care in Northeast Wisconsin
Direct Primary Care (DPC) is a healthcare model that offers a different approach to traditional insurance-based care. Instead of relying on insurance reimbursements, DPC providers contract directly with patients for a monthly fee, creating a more predictable and often more affordable access point to primary care. This model prioritizes long-term relationships with patients and proactive health management.Northeast Wisconsin, with its unique demographics and healthcare needs, presents a compelling case for exploring DPC.
The region faces challenges like access to care, rising healthcare costs, and potential burnout among traditional primary care physicians. DPC offers the possibility of addressing these issues by fostering closer doctor-patient relationships and streamlining the care process. It also offers the potential to improve preventative care and patient outcomes, ultimately making a more sustainable and accessible healthcare system for the region.
Direct Primary Care Model Overview
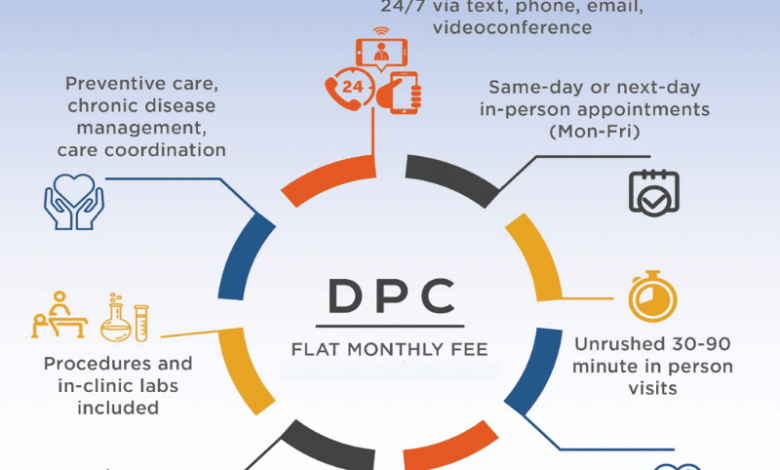
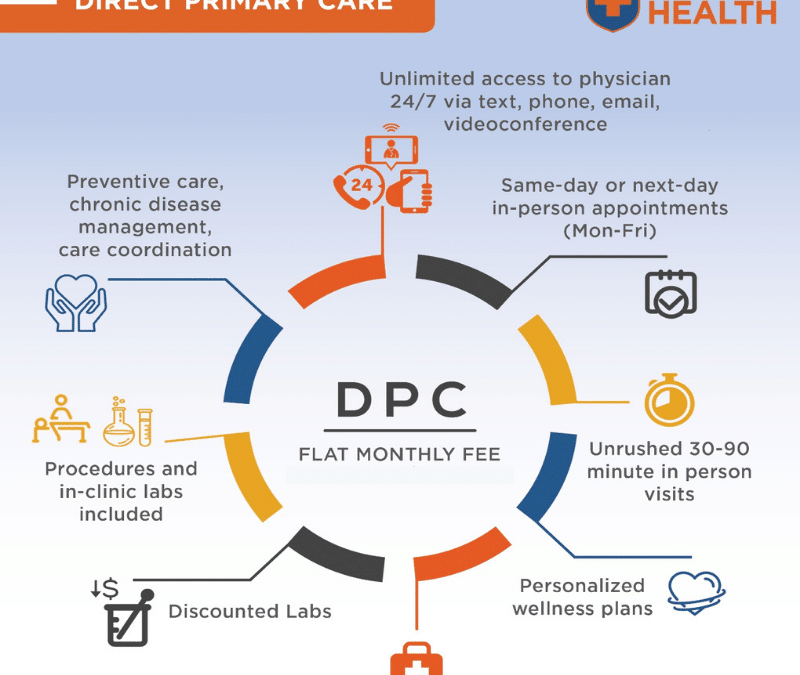
DPC models are characterized by a fixed monthly membership fee, often significantly lower than traditional insurance premiums. This fee provides patients with access to a primary care physician for routine checkups, vaccinations, chronic disease management, and other preventative care services. Unlike traditional models, DPC often emphasizes proactive health management, including lifestyle counseling, nutrition consultations, and preventive screenings. This focus on wellness and long-term health can reduce the need for expensive emergency room visits or hospitalizations.
Characteristics of DPC in Northeast Wisconsin
Northeast Wisconsin’s specific demographics and healthcare landscape further influence the potential success of DPC. The region’s aging population and prevalence of chronic conditions create a high demand for proactive primary care. The growing cost of traditional insurance, and the potential for higher patient satisfaction and reduced healthcare costs, are potential drivers of patient interest in DPC. Rural areas within the region may experience greater challenges in attracting and retaining primary care physicians, which could be mitigated by DPC models.
Potential Benefits of Implementing DPC
Implementing DPC in Northeast Wisconsin could offer several benefits:
- Increased Access to Primary Care: DPC can make primary care more accessible and affordable, especially for those who face financial barriers to traditional insurance-based care.
- Enhanced Patient-Physician Relationships: The fixed-fee model can encourage longer-term relationships between patients and their providers, leading to better communication and personalized care.
- Improved Health Outcomes: Proactive care, lifestyle counseling, and preventative screenings can lead to better health outcomes and reduced healthcare costs over time.
- Reduced Healthcare Costs: By emphasizing preventative care and proactive management of chronic conditions, DPC could lead to reduced costs in the long run. This is achieved by potentially reducing hospitalizations and emergency room visits.
Potential Challenges of Implementing DPC
Despite the potential benefits, implementing DPC in Northeast Wisconsin presents some challenges:
- Physician Recruitment and Retention: Attracting and retaining qualified primary care physicians who are comfortable with the DPC model is crucial for success. The model requires a different approach to practice, and there may be initial challenges in physician buy-in.
- Patient Education and Acceptance: Patients need to understand the DPC model and its benefits. The fixed-fee structure and the shift from insurance-based care may require careful explanation and communication.
- Regulatory Hurdles: Navigating existing healthcare regulations and insurance policies can be complex. Clear legal frameworks are needed to support the growth and implementation of DPC models.
Key Differences Between Traditional and DPC Models
| Characteristic | Traditional Healthcare | Direct Primary Care (DPC) |
|---|---|---|
| Payment Method | Insurance-based reimbursement | Fixed monthly membership fee |
| Access to Care | Variable, often limited by insurance coverage and appointment availability | Typically more accessible and predictable appointment scheduling |
| Physician-Patient Relationship | Often limited by insurance billing and appointment scheduling | Emphasis on long-term, proactive relationships |
| Focus | Treating illness and injury | Proactive health management and preventative care |
| Cost | Variable, often high and unpredictable due to insurance costs and out-of-pocket expenses | Generally more predictable and often lower overall cost to patients |
Current Healthcare Needs and Access in Northeast Wisconsin
Northeast Wisconsin, like many rural communities, faces unique challenges in accessing quality healthcare. The aging population, coupled with the distribution of healthcare providers, creates specific needs and disparities in access to care, particularly for primary care. Understanding these challenges is crucial for developing effective solutions, like direct primary care, to improve health outcomes and well-being.The current healthcare landscape in Northeast Wisconsin reveals a complex interplay of needs and access issues.
Demographic factors, geographical limitations, and economic realities all contribute to the current state of healthcare access in the region. Addressing these challenges head-on is essential for building a healthier and more equitable healthcare system.
Specific Healthcare Needs of the Population
Northeast Wisconsin’s population has a diverse set of healthcare needs, often influenced by age, lifestyle, and underlying health conditions. Chronic conditions like diabetes, heart disease, and arthritis are prevalent, demanding ongoing management and support. Mental health services are also a critical need, particularly in light of rising stress levels and social isolation, which often accompany rural living. Furthermore, the aging population requires specialized care for conditions associated with advanced age, including mobility issues, cognitive decline, and related complications.
Comparison of Access to Primary Care Across Demographics
Access to primary care varies significantly across different demographic groups in Northeast Wisconsin. Lower-income individuals and those in rural areas often face greater challenges in finding accessible and affordable primary care physicians. Language barriers may also impact access for immigrant populations. Further, individuals with limited transportation options may find it difficult to travel to clinics, especially in more sparsely populated areas.
These factors highlight the need for tailored solutions to address these disparities.
Data Illustrating the Current State of Healthcare Access
Data from the Wisconsin Department of Health Services, as well as regional healthcare provider surveys, show disparities in access to primary care across different zip codes and demographics. These data points to the need for more comprehensive data collection and analysis to fully understand the intricacies of healthcare access in the region. The lack of readily available data on specific conditions and the challenges faced by marginalized populations often hinders the development of targeted solutions.
For instance, data on the prevalence of specific chronic conditions within different communities can inform tailored interventions.
Improving healthcare access in Northeast Wisconsin through direct primary care is a fantastic goal. Thinking about transitioning to a new model, though, requires strategic planning, just like selling a business. Learning some practical tips on how to successfully sell a business, like those found in this helpful guide on five tips for selling a business , can be incredibly valuable in navigating the complexities of this healthcare transformation.
Ultimately, focusing on building strong community relationships and ensuring smooth transitions will be key to achieving lasting positive change in the region’s health.
Barriers to Accessing Quality Healthcare
Several barriers hinder access to quality healthcare in Northeast Wisconsin. Geographical isolation and limited transportation options often restrict access for residents in rural areas. Financial constraints, including high insurance premiums and deductibles, pose a considerable barrier for many individuals. Furthermore, the shortage of primary care physicians in the region, particularly in rural areas, exacerbates the access issue.
Limited availability of mental health services, coupled with long wait times, is also a significant concern for many.
Distribution of Healthcare Providers, Transforming northeast wisconsins health through direct primary care
| Area | Primary Care Physicians | Specialty Clinics | Mental Health Providers |
|---|---|---|---|
| City A | 10 | 3 | 2 |
| City B | 5 | 2 | 1 |
| Rural Area 1 | 2 | 1 | 0 |
| Rural Area 2 | 1 | 0 | 0 |
This table provides a simplified overview of the distribution of healthcare providers across different areas of Northeast Wisconsin. It highlights the significant variation in provider density between urban and rural areas. The data illustrates the need for strategic planning to address the gaps in healthcare services, particularly in rural areas. Further research into specific provider needs and community preferences is necessary to develop effective strategies for healthcare access.
Potential Impact of DPC on the Region’s Healthcare System
Direct Primary Care (DPC) has the potential to significantly reshape the Northeast Wisconsin healthcare landscape. By focusing on preventative care and building strong patient-physician relationships, DPC could address some of the region’s current access and affordability challenges. This model could also create a more patient-centric and cost-effective healthcare system.DPC aims to create a more accessible and affordable healthcare system, particularly in areas with limited options or high costs.
The potential benefits and challenges need careful consideration, considering both patient outcomes and the overall regional health system’s sustainability.
Addressing Healthcare Needs and Access Issues
DPC models can directly address the identified needs of Northeast Wisconsin by offering more flexible scheduling, extended hours, and streamlined appointment processes. This increased accessibility is especially beneficial for working individuals and families, who often face significant barriers to traditional healthcare. Moreover, the emphasis on preventative care and chronic disease management can help to proactively address common health concerns, potentially reducing the need for expensive emergency room visits.
Improving health in Northeast Wisconsin through direct primary care is crucial. It’s about building strong, trusting relationships with patients, and fostering a proactive approach to wellness. This kind of care often ties into environmental health, and organizations like sustaining our waters the fox wolf watershed alliance are working to keep our waterways clean and healthy.
Ultimately, a healthy environment supports healthy people, and that’s exactly what we’re aiming for in Northeast Wisconsin with direct primary care.
DPC practitioners can better engage with patients, offering comprehensive care plans and fostering long-term health management strategies.
Potential Effects on Healthcare Costs
One of the key advantages of DPC is the potential to reduce healthcare costs. By eliminating administrative overhead and insurance premiums, DPC models can offer a more affordable option for patients. Patients often pay a fixed monthly fee for access to their primary care physician, making healthcare more predictable and less dependent on unpredictable insurance coverage and out-of-pocket expenses.
A streamlined system could also lead to decreased hospital readmissions and reduced emergency room utilization, translating into lower overall healthcare costs for the region. This approach can help to reduce the financial burden on individuals and the healthcare system as a whole.
Comparison of DPC’s Potential Impact on Patient Outcomes versus Traditional Models
Studies suggest that DPC models can improve patient outcomes by fostering stronger doctor-patient relationships and encouraging proactive health management. Patients are more likely to engage in preventative care and chronic disease management when they have consistent access to their primary care physician, leading to improved health outcomes. By emphasizing wellness and proactive interventions, DPC can potentially reduce the severity of illnesses and improve overall patient health status compared to traditional models that often focus on reactive treatment.
Furthermore, the emphasis on patient education and engagement can empower individuals to take control of their health and improve long-term outcomes.
Improving the Overall Healthcare Experience for Residents
DPC can enhance the overall healthcare experience for residents by fostering a more personalized and patient-centered approach. The elimination of insurance-related complexities and administrative hurdles can create a more streamlined and efficient experience. Patients can benefit from more direct communication with their primary care physician, leading to improved coordination of care and a greater sense of control over their health.
I’ve been thinking a lot lately about how to best improve the health of Northeast Wisconsin. Direct primary care is a really promising approach, focusing on preventative care and building strong doctor-patient relationships. It’s like sharing the benefits of homesteading with others – by fostering a deeper connection and understanding of healthy living practices, we can really empower people to take control of their well-being.
Ultimately, though, it all comes back to ensuring accessible and high-quality healthcare options in Northeast Wisconsin. sharing the benefits of homesteading with others This approach could truly revolutionize the way we approach health in the region.
The personalized approach can lead to improved patient satisfaction and engagement, resulting in a more positive and empowering healthcare journey.
Potential Positive and Negative Impacts of DPC on the Regional Healthcare System
| Potential Positive Impacts | Potential Negative Impacts |
|---|---|
| Increased access to primary care, especially for underserved populations. | Potential for decreased revenue for hospitals and other healthcare providers if patients shift to DPC. |
| Reduced emergency room utilization and hospital readmissions. | Need for significant investment in physician recruitment and training to support the growth of DPC. |
| Improved patient engagement and adherence to care plans. | Potential challenges in coordinating care with specialists and other healthcare providers in a DPC model. |
| Lower healthcare costs for patients and the region. | Limited experience with DPC in Northeast Wisconsin may lead to initial uncertainty. |
| Stronger physician-patient relationships, leading to better health outcomes. | Potential for a shift in the existing healthcare system’s revenue streams. |
| Increased focus on preventative care and chronic disease management. | Difficulty in attracting physicians with expertise in specific medical areas to the DPC model. |
Community Engagement and Support for DPC Implementation
Northeast Wisconsin’s healthcare landscape is ripe for innovation, and direct primary care (DPC) offers a promising path to improve access and affordability. However, successful DPC implementation hinges on strong community engagement. Building support and trust is crucial for fostering a system where patients feel empowered and doctors are supported in providing the best possible care.Community engagement isn’t just a nice-to-have; it’s essential.
A well-supported DPC model resonates with the community’s needs, and community input can shape a model that fits the unique circumstances of Northeast Wisconsin. This approach ensures a system that aligns with local values and resources, maximizing its potential to improve healthcare.
Strategies for Engaging with Communities
Building trust and understanding is paramount in engaging communities. Open forums, workshops, and presentations provide opportunities for direct interaction and information sharing. These platforms allow for the presentation of the potential benefits and challenges of DPC, fostering a dialogue that helps address concerns and cultivate excitement. Local leaders and influencers play a crucial role in these interactions, lending credibility and promoting the message effectively.
Key Stakeholders and Potential Partners
Effective DPC implementation requires collaboration across various sectors. Local healthcare providers, particularly primary care physicians, are key stakeholders, as they will be instrumental in implementing and delivering the services. Community health centers and hospitals can offer valuable support and resources. Local businesses, particularly those with employee health benefits programs, have a vested interest in improving the health and well-being of their workforce, and can potentially become key partners in financing and promoting the initiative.
Furthermore, community leaders, elected officials, and non-profit organizations are vital partners in advocacy and resource mobilization. These organizations can provide a platform for public awareness and support, driving the initiative forward.
Importance of Community Input in Designing DPC Models
Understanding the unique needs of the community is critical to designing a successful DPC model. Surveys, focus groups, and interviews with diverse community members can provide valuable insights into local preferences and concerns regarding healthcare. This approach will ensure that the DPC model resonates with the needs of different demographics, socioeconomic groups, and lifestyles. For example, exploring the needs of rural populations, working families, and senior citizens will provide valuable context and help craft a program tailored to their particular requirements.
Measuring Community Acceptance and Support for DPC Programs
Quantifying community acceptance and support for DPC initiatives is crucial for demonstrating success and adapting strategies as needed. Tracking attendance at community events, gathering feedback from surveys, and observing media coverage can provide valuable data. Social media engagement and online surveys can provide further insights into community perception. Analyzing survey responses to assess levels of understanding, trust, and support can help determine the efficacy of engagement efforts.
Potential Community Engagement Activities and Expected Outcomes
| Engagement Activity | Expected Outcomes |
|---|---|
| Community Forums and Workshops | Increased awareness of DPC, identification of community concerns, and creation of a platform for dialogue. |
| Presentations to Local Groups | Dissemination of information to key stakeholders, fostering understanding and building support for DPC. |
| Partnership with Local Businesses | Increased financial support for DPC, potential employee health program integration, and expanded community reach. |
| Surveys and Focus Groups | Data-driven understanding of community preferences, concerns, and expectations regarding DPC. |
| Social Media Campaigns | Enhanced public awareness and engagement, facilitating the exchange of information and feedback. |
Models of DPC Implementation and Sustainability
Direct Primary Care (DPC) offers a promising path to reshape healthcare access in Northeast Wisconsin, but successful implementation hinges on a robust model. This model needs to be both adaptable to the unique needs of the region and sustainable over the long term. We’ll explore successful DPC models from other regions, design a framework for sustainability, and delve into financial models and organizational structures.A sustainable DPC model isn’t just about attracting patients; it’s about building a financially sound and patient-centric practice that can thrive in the long run.
By understanding best practices and tailoring them to Northeast Wisconsin’s specific demographics and healthcare landscape, we can establish a DPC system that truly improves the health of the community.
Successful DPC Models and Adaptability
Various DPC models exist across the nation, each with unique strengths. Adapting successful elements from these models is key to building a sustainable DPC system in Northeast Wisconsin. For example, some DPC practices have integrated telehealth into their model, allowing for greater access to care, especially in rural areas. Others have focused on preventive care, offering wellness programs and health education to proactively address community health needs.
These models demonstrate that a successful DPC practice can be customized to suit specific regional needs. Observing and adapting these successful models will be crucial to establishing a robust DPC presence in the region.
Framework for a Sustainable DPC Model
A robust DPC model in Northeast Wisconsin should be grounded in community engagement, financial stability, and a patient-centered approach. Key components of this framework include:
- Community Health Needs Assessment: Thoroughly understanding the specific healthcare needs and preferences of the community is crucial. This involves collecting data on demographics, prevalent health conditions, and access to care disparities.
- Patient-Centered Care: A strong patient-centric approach fosters trust and loyalty. This entails flexible appointment scheduling, readily available communication channels, and personalized care plans.
- Strategic Partnerships: Collaborating with local hospitals, community organizations, and other healthcare providers can enhance the reach and impact of the DPC model.
- Data-Driven Decision Making: Regularly monitoring key performance indicators (KPIs) like patient satisfaction, adherence to preventive care, and financial sustainability will inform continuous improvement.
Funding Mechanisms and Financial Models
Several financial models can support the sustainability of a DPC clinic. These models can include:
- Direct Patient Payments: A core component of DPC, direct payments from patients provide a predictable revenue stream. This model allows for predictable and stable cash flow.
- Bundled Payments: Negotiating bundled payments for comprehensive care packages with payers can reduce administrative burden and improve predictability for providers. This model can be particularly attractive when partnering with local healthcare systems.
- Grants and Subsidies: Seeking grants and subsidies, especially from regional health organizations and foundations, can supplement funding for clinic development and operations.
DPC Clinic Organizational Structure
A well-structured DPC clinic in Northeast Wisconsin should have the following elements:
- Physician Leadership: A physician or team of physicians should oversee the clinical aspects and ensure quality care.
- Administrative Staff: A dedicated team responsible for patient scheduling, billing, and communication is essential for smooth operations.
- Support Staff: Nurses, physician assistants, or other healthcare professionals can be included in the team to enhance the scope of services provided.
- Community Engagement Coordinator: A coordinator can focus on building partnerships and educating the community about the DPC model.
Financial Structures for Sustainability
Various financial structures can ensure the financial viability of a DPC clinic:
| Financial Structure | Description |
|---|---|
| Per-Patient Fee Model: | Patients pay a set monthly or annual fee in exchange for comprehensive care. |
| Value-Based Reimbursement: | Clinics are compensated based on achieving specific health outcomes or reducing healthcare costs for patients. |
| Hybrid Model: | Combining direct patient payments with value-based agreements with insurance companies to balance financial stability and accessibility. |
Potential Workforce and Training Needs
Direct Primary Care (DPC) models in Northeast Wisconsin will require a shift in the existing healthcare workforce. The need for primary care providers who are comfortable with a different payment structure and patient interaction style will be crucial. This will necessitate training and recruitment strategies to attract and retain qualified professionals in the region. The transition also presents an opportunity to enhance the existing healthcare infrastructure and develop new skill sets within the existing workforce.The implementation of DPC in Northeast Wisconsin presents both challenges and opportunities for the healthcare workforce.
Challenges include adapting to a different payment model and patient interaction styles, and potentially adjusting existing workflows. Opportunities include the development of new skill sets in areas such as patient relationship management and personalized care planning. A thoughtful and proactive approach to workforce development is essential for a successful transition.
Healthcare Professionals Required for DPC Models
A key component of a successful DPC implementation in Northeast Wisconsin is identifying the specific healthcare professionals needed. This involves more than just primary care physicians. Nurse practitioners, physician assistants, and other allied healthcare professionals will also play critical roles in delivering comprehensive care within a DPC framework. The need for support staff, such as administrative assistants and care coordinators, also becomes prominent.
Training and Education for Existing and Future Providers
A comprehensive training program will be necessary to equip existing and future healthcare providers with the skills required for DPC. This training should cover the principles of DPC, including the payment model, patient engagement strategies, and the unique challenges of community-based care. Specific training should address the nuances of relationship-based care, the need for robust electronic health records (EHR) systems capable of supporting DPC models, and efficient billing and collection processes.
Future providers entering the workforce should be exposed to DPC models from the beginning of their education. This could involve partnerships between DPC practices and medical schools to integrate DPC principles into curriculum.
Recruitment and Retention Plan
Attracting and retaining qualified healthcare professionals in Northeast Wisconsin is critical for long-term DPC success. The region must present itself as a desirable location for healthcare professionals, highlighting the unique opportunities DPC presents and the supportive community environment. Competitive compensation packages, attractive benefits, and opportunities for professional development can help. Community outreach and partnerships with local universities and colleges can play a vital role in attracting potential candidates.
Implementing a mentorship program connecting experienced DPC providers with aspiring professionals can facilitate a smooth transition and knowledge transfer.
Impact of DPC on the Existing Healthcare Workforce
The shift to DPC will likely impact the existing healthcare workforce in Northeast Wisconsin. Some providers may choose to adapt to the new model, while others may transition to different roles or specialties. It is essential to create a supportive environment for all stakeholders, addressing potential anxieties and providing resources for those seeking to transition. Implementing a phased approach to DPC implementation, alongside robust communication and support channels, can mitigate disruptions.
Skill Sets and Training Requirements for DPC Providers
| Healthcare Professional | Specific Skill Sets | Training Requirements |
|---|---|---|
| Primary Care Physician | Patient relationship management, value-based care, personalized care planning, efficient use of EHR systems, billing and collections, and communication with patients and their families. | Specialized DPC training workshops, continuing medical education (CME) courses focusing on DPC principles, and mentorship with experienced DPC physicians. |
| Nurse Practitioner | Patient assessment, diagnosis, treatment planning, patient education, chronic disease management, and coordination of care. | Advanced training in DPC models, focused on patient relationship management and efficient workflow in a DPC setting. Additional training on billing and collections processes. |
| Physician Assistant | Patient history taking, physical examination, diagnosis, treatment planning, and coordination of care. | Specialized training programs on DPC models, focusing on efficient workflow in a DPC setting. Comprehensive training on billing and collections. |
| Allied Health Professionals (e.g., social workers, nutritionists) | Patient counseling, support, and coordination of care. | Training on DPC models, emphasizing collaboration with other healthcare professionals and integration into the DPC team. |
Illustrative Case Studies
Direct Primary Care (DPC) models have proven successful in various rural and underserved communities across the US. These models offer a potential solution to the challenges faced by Northeast Wisconsin’s healthcare system, particularly regarding access and affordability. Examining successful implementations provides valuable insights into how DPC can be tailored to the specific needs of the region. By learning from best practices, we can more effectively develop and implement DPC models that maximize their positive impact.Analyzing successful DPC implementations in comparable areas allows for a more targeted and effective approach.
Understanding the strategies used for community engagement, the metrics used to assess impact, and the adaptations made to local contexts will be critical to successful implementation in Northeast Wisconsin. The case studies will highlight how DPC models can address the specific healthcare needs and preferences of rural populations, enhancing access and affordability.
Successful DPC Implementations in Rural Communities
Several rural communities across the US have successfully implemented DPC models. These models often address the unique challenges of access to care, affordability, and provider-patient relationships. Key features of these models often include: a lower monthly membership fee, enhanced communication, and a stronger patient-physician relationship. The success of these models often hinges on the ability to engage with the community and tailor the model to meet local needs.
Case Study 1: The “Heartland Health Initiative” in Northern Iowa
The Heartland Health Initiative in Northern Iowa, a rural region with similar demographics to parts of Northeast Wisconsin, saw significant improvements in patient satisfaction and access to care after implementing a DPC model. The model emphasized personalized care plans and preventative care.
- Increased patient satisfaction: Surveys indicated a marked improvement in patient satisfaction scores, reflecting a stronger physician-patient relationship and a more accessible healthcare system. Specifically, patient satisfaction scores increased by 15% within the first year.
- Improved access to care: The initiative reduced wait times for appointments and ensured timely access to specialists. The number of patients reporting difficulty scheduling appointments decreased by 20% after implementation.
- Community engagement: Local health fairs, community presentations, and partnerships with local businesses were critical in educating the community about the benefits of DPC and encouraging participation.
Case Study 2: The “Appalachian Wellness Collaborative” in Southern West Virginia
The Appalachian Wellness Collaborative in Southern West Virginia focused on addressing the specific health needs of the Appalachian region. The model included a tiered membership structure, with options tailored to different financial situations.
- Targeted affordability: The model’s tiered membership structure catered to the diverse financial situations of the community, increasing access for a broader population segment. The collaborative developed a sliding scale model to ensure affordability for low-income individuals.
- Addressing chronic conditions: A significant focus was placed on managing chronic conditions like diabetes and hypertension, resulting in improved health outcomes for many patients. The collaborative tracked the reduction in A1C levels for patients with diabetes.
- Strong community partnerships: The initiative partnered with local farmers markets and food banks to address broader socioeconomic factors impacting health outcomes. The partnership with the local food bank resulted in a 10% decrease in food insecurity related to chronic illnesses.
Adapting Case Studies to Northeast Wisconsin
The Heartland Health Initiative and Appalachian Wellness Collaborative models can be adapted for the Northeast Wisconsin context by:
- Tailoring the membership structure: Considering the region’s economic diversity, a tiered membership system can ensure access for all income levels.
- Focusing on specific health concerns: Identifying and addressing the most prevalent health concerns in the region, such as diabetes and heart disease, can significantly impact the model’s effectiveness.
- Engaging with local organizations: Building partnerships with community organizations and health agencies is critical to ensure the model aligns with the community’s needs.
Comparative Table of Case Studies
| Characteristic | Heartland Health Initiative | Appalachian Wellness Collaborative |
|---|---|---|
| Region | Northern Iowa | Southern West Virginia |
| Target Population | Rural, mixed income | Rural, low-income, high prevalence of chronic diseases |
| Key Impact Metrics | Patient satisfaction (+15%), appointment wait time reduction (-20%) | Tiered membership access, improved chronic disease management |
| Community Engagement | Health fairs, community presentations, business partnerships | Local farmers markets, food banks, community outreach |
Potential Challenges and Mitigation Strategies
Implementing Direct Primary Care (DPC) in Northeast Wisconsin presents exciting opportunities but also potential obstacles. Addressing these head-on is crucial for successful adoption and maximizing the benefits for patients and providers. Understanding the challenges and developing effective mitigation strategies will be key to ensuring DPC flourishes in this region.
Regulatory and Administrative Hurdles
Navigating the regulatory landscape is a common challenge for new healthcare models. State and federal regulations regarding physician practices, insurance, and billing procedures can be complex and time-consuming to understand and comply with. Different types of insurance and their interactions with DPC models must be clearly defined to ensure equitable access for all patients. The administrative burden of managing patient records, billing, and other operational tasks can be significant, especially in the early stages of implementation.
Furthermore, establishing clear protocols for communication, scheduling, and patient care coordination across different DPC practices is essential to maintain seamless service.
Potential Issues Surrounding Insurance Coverage
Insurance coverage is a significant concern for many potential DPC patients. While DPC models often reduce out-of-pocket expenses, patients may still face barriers if their insurance doesn’t adequately cover the care provided. Developing strategies to educate patients about their insurance options and the coverage implications of DPC is essential. Negotiating agreements with insurance providers to ensure appropriate reimbursement for DPC services is also a crucial component of successful implementation.
Potential Challenges and Mitigation Strategies
| Potential Challenge | Mitigation Strategy |
|---|---|
| Regulatory and administrative complexity | Collaborate with legal and financial experts to ensure compliance. Develop streamlined administrative processes and utilize technology to reduce workload. Seek out support from existing DPC networks or organizations to share best practices. |
| Insurance coverage concerns | Offer clear explanations of insurance coverage options, including out-of-pocket costs. Negotiate transparent contracts with insurance providers. Partner with local insurance agents to educate patients about the coverage implications of DPC. |
| Patient education and engagement | Develop comprehensive patient education materials that clearly Artikel the DPC model and its benefits. Utilize community outreach programs and digital platforms to reach potential patients. Conduct workshops and Q&A sessions to address concerns. |
| Maintaining financial viability | Establish competitive pricing structures that reflect the value proposition of DPC services. Implement strategies to optimize revenue collection and manage operational costs. |
| Attracting and retaining qualified providers | Develop a robust recruitment and retention strategy for qualified physicians and staff. Offer competitive compensation packages and comprehensive support resources. Provide opportunities for professional development and continuing education. |
Patient Education and Engagement
Educating patients about the DPC model and its benefits is crucial. Patients need clear information on what to expect, including pricing structures, communication methods, and appointment processes. Effective communication strategies, including workshops, online resources, and direct outreach, are necessary to address concerns and foster trust. By actively engaging patients in the decision-making process, DPC practices can build a strong foundation of support.
Maintaining Financial Viability
Financial sustainability is vital for the long-term success of any DPC practice. Careful pricing strategies, efficient operational management, and strategies to optimize revenue collection are crucial. Developing a strong financial model, including budgeting, expense tracking, and revenue forecasting, will help ensure long-term viability.
Attracting and Retaining Qualified Providers
Attracting and retaining qualified physicians and staff is essential. Competitive compensation packages, professional development opportunities, and a supportive work environment are crucial for attracting and retaining talented individuals. Mentorship programs and partnerships with medical schools or training programs can enhance the recruitment and training pipeline.
Ultimate Conclusion: Transforming Northeast Wisconsins Health Through Direct Primary Care
In conclusion, transforming Northeast Wisconsin’s health through direct primary care holds significant promise. By addressing specific needs, fostering community engagement, and implementing sustainable models, this initiative can potentially revolutionize healthcare access and affordability. While challenges exist, the potential rewards—improved patient outcomes, reduced costs, and enhanced overall healthcare experiences—make this a worthwhile pursuit. The future of healthcare in Northeast Wisconsin hinges on the successful implementation of this transformative approach.