DCMC to Open DirectCare Non-Emergency Care
Dcmc to open directcare non emergency care – DCMC to open DirectCare non-emergency care is a significant shift in healthcare delivery. This transition promises streamlined access to crucial non-emergency services, offering patients a more convenient and efficient pathway to care. The change involves a complete overhaul, including the transfer of patient information, provider integration, and enhanced data security. Understanding the specifics of this transition is crucial for both patients and healthcare providers to navigate the new system effectively.
This detailed guide delves into the process, outlining the steps involved, potential challenges, and solutions. We’ll cover everything from patient registration and access to data management and security protocols, ultimately aiming to demystify the entire process for a smoother transition.
Overview of DirectCare Non-Emergency Care
DirectCare Non-Emergency Care offers a convenient and accessible alternative to traditional emergency room visits for patients needing medical attention outside of true emergencies. This streamlined approach prioritizes prompt and quality care while minimizing wait times and potential costs.This system is designed to provide a more efficient and patient-centric experience, offering a wide array of services for a variety of conditions.
It focuses on reducing the burden on emergency departments, ensuring timely access to appropriate care for those who don’t require immediate life-saving interventions.
Patient Experience within DirectCare
The DirectCare experience typically involves an initial contact, often through a phone call or online portal. This allows patients to describe their symptoms and concerns. Subsequently, they may be directed to a facility equipped with appropriate medical professionals, who will conduct a thorough assessment and develop a tailored treatment plan. This process often includes testing, observation, and if necessary, follow-up appointments to ensure the patient’s well-being.
Types of Services Offered
DirectCare Non-Emergency Care provides a range of services, encompassing routine checkups, treatment for acute illnesses, minor injuries, and follow-up care for existing conditions. Examples include: treatments for colds, flu, and other minor illnesses; wound care for cuts and scrapes; management of chronic conditions; and prescription refills. The services offered are tailored to meet the needs of a broad spectrum of patients, addressing conditions ranging from common ailments to more complex health issues.
DCMC is opening direct care non-emergency services, which is fantastic news. This aligns well with the recent redesignation of the Stevens Points Breast Care Center, demonstrating a commitment to community health and accessible care. The focus on improving access to quality healthcare, like the new direct care options at DCMC, is essential for the well-being of our community.
stevens points breast care center receives redesignation This expanded direct care network at DCMC is a step in the right direction.
Comparison to Traditional Emergency Room Visits
| Characteristic | DirectCare Non-Emergency Care | Traditional Emergency Room Visit |
|---|---|---|
| Wait Time | Generally shorter wait times, often within an hour or less. | Potentially significantly longer wait times, depending on demand and acuity of cases. |
| Cost | Typically lower cost compared to an ER visit. | Potentially higher cost, especially for non-life-threatening conditions. |
| Accessibility | Convenient access through phone calls, online portals, or walk-in appointments at designated facilities. | Often requires immediate arrival at a facility, potentially involving travel time. |
| Service Focus | Focused on non-life-threatening conditions and illnesses. | Focused on life-threatening conditions and emergencies. |
| Staffing | Staffed with qualified medical professionals, often nurse practitioners and physician assistants, with expertise in managing a wide range of conditions. | Staffed with a diverse team of specialists, including emergency physicians, nurses, and technicians, equipped to handle various emergencies. |
Transitioning from DCMC to DirectCare
Navigating the transition from DirectCare Management Center (DCMC) to DirectCare Non-Emergency Care requires a smooth and well-defined process. This involves not only transferring patient data but also ensuring a seamless experience for both patients and healthcare providers. This detailed guide Artikels the steps, potential challenges, and mitigating strategies for a successful transition.
Patient Information Transfer Process
The transfer of patient information from DCMC to DirectCare is crucial for continuity of care. This process involves meticulous data extraction, validation, and secure transfer to ensure accuracy and minimize delays in patient care. Specific protocols are in place to ensure data integrity and compliance with privacy regulations. This careful process ensures that patient information is not only transferred but also properly formatted and accessible within the DirectCare system.
Steps for Patients
Patients need clear communication and support throughout the transition. This includes receiving instructions on how to access their DirectCare account, if applicable. A dedicated support team is available to address any questions or concerns during this period. Patients will also receive notifications and instructions about accessing their records, and any necessary paperwork.
Steps for Healthcare Providers
Healthcare providers will need to familiarize themselves with the new DirectCare system. Training programs are essential to ensure proficiency in using the new platform and navigating the patient information. This training includes understanding the new workflows, data entry procedures, and accessing patient records within the DirectCare system. They also need access to updated protocols, resources, and contact information for support.
Potential Challenges and Mitigation Strategies
Data migration projects can present challenges. Potential issues may include data inconsistencies, technical glitches, or user difficulties. To mitigate these challenges, robust testing and validation procedures are crucial before the transition. A dedicated help desk will be available for support and troubleshooting. Comprehensive training programs, detailed documentation, and communication channels will help mitigate user confusion.
Required Documentation for Patient Transfer
The following table Artikels the essential documentation required for a successful patient transfer:
| Document Category | Description |
|---|---|
| Patient Demographics | Name, Date of Birth, Address, Contact Information, Insurance Information |
| Medical History | Past medical conditions, diagnoses, allergies, medications |
| Treatment Records | Previous treatment plans, procedures, and results |
| Immunization Records | Vaccination history, including dates and types of vaccines |
| Lab Results | Recent lab results, including values and dates |
| Imaging Reports | Imaging reports (X-rays, CT scans, MRIs), including dates and findings |
Patient Access and Registration
Getting registered for DirectCare Non-Emergency Care is a straightforward process designed for seamless access to quality healthcare. This section Artikels the steps involved in registering and accessing DirectCare services, highlighting the importance of accurate patient identification and verification. Understanding these procedures will empower you to utilize DirectCare’s services effectively.
Registration Process
The registration process for DirectCare Non-Emergency Care is designed to be efficient and user-friendly. Patients can choose from various methods to complete their registration, ensuring accessibility for diverse needs. These options include online registration, phone-based registration, or in-person registration at designated locations. Each method offers a unique approach to the registration process, making it suitable for different patient preferences and circumstances.
Methods of Access
DirectCare offers multiple avenues for accessing services, catering to diverse patient preferences and needs. Patients can access DirectCare through a user-friendly online portal, dedicated phone lines, or by visiting a designated physical location. The choice of access method is entirely up to the patient, considering factors such as convenience and personal comfort.
- Online Registration: This method allows patients to complete the registration process from the comfort of their homes, using a computer or mobile device. This option is particularly convenient for those who prefer self-service and prefer not to interact with a phone or in-person staff.
- Phone-Based Registration: Patients can register by contacting DirectCare’s dedicated phone lines. This option is ideal for those who prefer a direct interaction with a representative, or those who may find online registration challenging.
- In-Person Registration: Patients can visit a designated DirectCare location for in-person registration. This option is advantageous for those who prefer a face-to-face interaction with a registration staff member or those who may require additional assistance or support.
Patient Identification and Verification
Accurate patient identification and verification are critical for ensuring the delivery of appropriate and personalized care. DirectCare employs secure protocols to verify patient information, protecting sensitive data and maintaining the privacy of each individual. This process safeguards the patient’s medical records and ensures the correct provision of services. Robust verification measures help ensure patient information is precise and current.
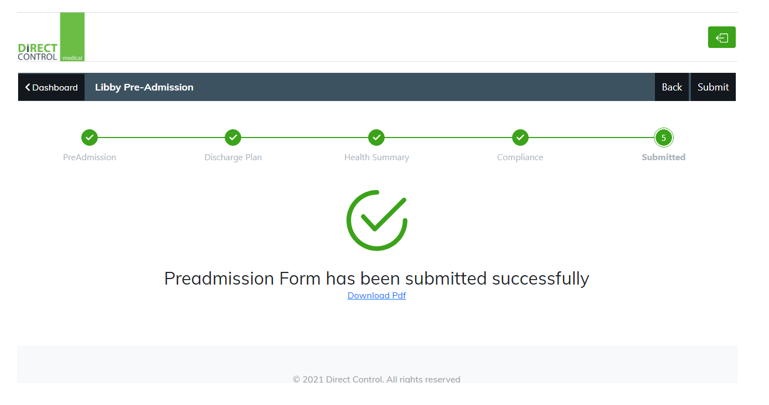
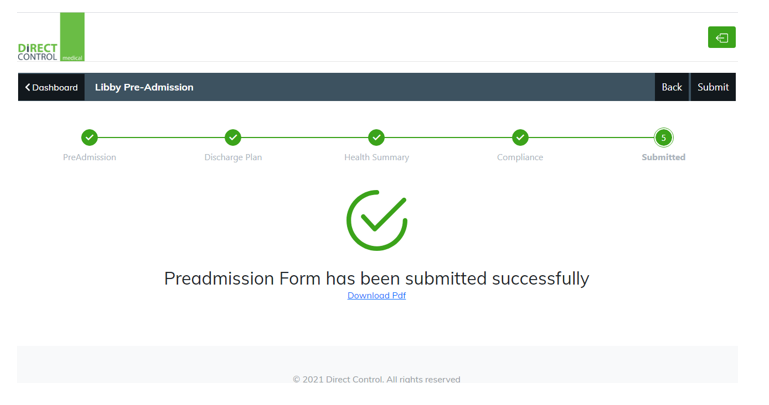
Online Registration Steps
The following table Artikels the steps involved in registering online for DirectCare Non-Emergency Care.
| Step | Action |
|---|---|
| 1 | Visit the DirectCare website and locate the registration portal. |
| 2 | Provide necessary personal information, including name, date of birth, address, and contact details. |
| 3 | Select the appropriate healthcare plan and complete the required registration forms. |
| 4 | Review the provided information for accuracy and submit the registration form. |
| 5 | Receive a confirmation email with a unique login ID and password. |
| 6 | Use the provided credentials to log into the DirectCare portal and access services. |
Provider Integration and Communication
Transitioning to DirectCare requires a smooth integration process for all healthcare providers. This section details the steps involved in ensuring a seamless transition, focusing on effective communication protocols between providers currently using DCMC and those utilizing DirectCare. This crucial aspect facilitates continuity of care and ensures a positive patient experience.
Integration Process for Healthcare Providers
The transition to DirectCare involves a phased approach for providers. Initial steps include comprehensive training on the DirectCare platform, including functionalities, data entry protocols, and security measures. Providers will receive access to online resources, FAQs, and dedicated support channels. This ensures they can efficiently utilize the new system. A dedicated team will assist providers with any questions or issues that may arise during the onboarding process.
Communication Protocols Between Providers
Effective communication is paramount for continuity of care. Communication protocols between DirectCare and DCMC providers are established to ensure timely and accurate information exchange. A critical component involves a secure, real-time data exchange system between the two platforms. This system will enable providers to access relevant patient information, ensuring accurate diagnoses and treatment plans. The protocols also include established processes for escalating issues or concerns.
Role of DirectCare in Facilitating Provider Communication
DirectCare plays a central role in facilitating seamless communication between providers. The system incorporates features designed for efficient communication, including secure messaging, shared patient portals, and automated alerts. This technology enables providers to exchange crucial information, such as test results, medication histories, and treatment plans, in a secure and timely manner. Real-time updates ensure providers are aware of the most current information regarding a patient’s condition.
DirectCare Communication Channels
The DirectCare system utilizes various communication channels to facilitate seamless provider interaction. These channels ensure efficient and secure data exchange between providers.
| Communication Channel | Description | Example Use Case |
|---|---|---|
| Secure Messaging | Encrypted messaging platform for secure exchange of critical information, such as test results, diagnoses, and treatment plans. | Dr. Smith sends Dr. Garcia the results of a recent MRI scan for a patient. |
| Shared Patient Portals | Secure online platforms for providers to access and update patient information. | Nurse Jones updates the patient’s medication list in the shared portal. |
| Automated Alerts | Notifications for critical updates or changes in patient status. | The system sends an alert to all providers when a patient’s blood pressure drops below a critical threshold. |
| Real-time Data Exchange | A secure system that enables immediate access to updated patient information across providers. | Dr. Brown immediately sees that Dr. Davis has prescribed a new medication for a patient. |
Data Management and Security
DirectCare prioritizes the confidentiality and security of patient data. This is paramount to building trust and ensuring patient well-being. Robust data management systems and stringent security protocols are implemented to safeguard sensitive information. This section details the strategies employed by DirectCare to maintain the integrity and privacy of patient records.DirectCare employs a comprehensive approach to managing patient data, integrating multiple layers of security controls to protect sensitive information.
The system is designed to comply with all relevant data privacy regulations and industry best practices. This includes secure data storage, access controls, and regular security audits.
Patient Data Management, Dcmc to open directcare non emergency care
DirectCare utilizes a centralized electronic health record (EHR) system to store and manage patient data. This system ensures data integrity, accessibility, and interoperability. The system is designed to accommodate a large volume of data while maintaining efficient retrieval and analysis capabilities. Data is organized logically, allowing for easy searching and retrieval by authorized personnel. This structured approach supports efficient care coordination and improves the overall patient experience.
Security Protocols
DirectCare employs a multi-layered approach to data security, encompassing several key protocols. These protocols are designed to protect patient data from unauthorized access, use, disclosure, alteration, or destruction. This includes robust access controls, regular security audits, and encryption of sensitive data. Furthermore, DirectCare adheres to strict guidelines for user authentication, data backups, and disaster recovery planning. This comprehensive approach safeguards patient information throughout its lifecycle.
Data Privacy Regulations
DirectCare adheres to all applicable data privacy regulations, including HIPAA (Health Insurance Portability and Accountability Act) in the United States. These regulations Artikel strict guidelines for the use and disclosure of protected health information (PHI). DirectCare’s policies and procedures are aligned with these regulations to ensure compliance and protect patient privacy. The organization regularly reviews and updates its policies to remain compliant with evolving regulations.
Comparison of Data Security Measures
| Feature | DCMC | DirectCare |
|---|---|---|
| Data Encryption | Data stored using industry-standard encryption methods, but specific methods not detailed publicly. | All sensitive patient data is encrypted both in transit and at rest using AES 256-bit encryption. |
| Access Control | Multi-layered access control system, but details of authentication and authorization are not publicly disclosed. | Robust multi-factor authentication (MFA) system with role-based access controls. All user access is logged and monitored. |
| Data Backup and Recovery | Regular backups, but frequency and recovery time objective (RTO) not specified. | Automated, encrypted backups are performed daily and stored in secure offsite locations. RTO for recovery is 24 hours. |
| Security Audits | Periodic security audits performed, but frequency and scope not detailed. | Regular penetration testing, vulnerability assessments, and security audits are conducted quarterly by independent security firms. |
This table highlights the key differences in data security measures between DCMC and DirectCare. DirectCare’s enhanced protocols reflect a commitment to maintaining the highest levels of patient data protection.
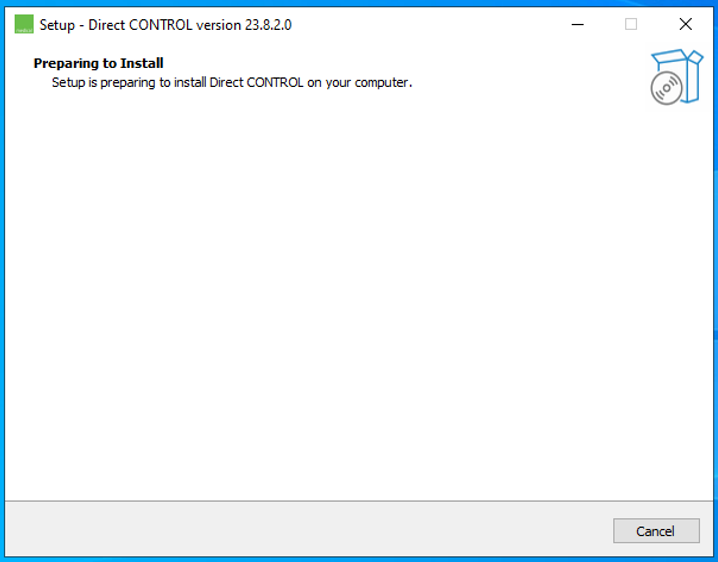
System Usability and Functionality
The DirectCare system’s usability and functionality are crucial for a smooth transition and positive patient experience. This section details the system’s features, focusing on its user-friendliness and functionality from both patient and provider perspectives. Understanding the technical aspects is also key for effective implementation and maintenance.The DirectCare system is designed with a user-centered approach, prioritizing ease of navigation and intuitive interfaces.
This ensures both patients and providers can quickly learn and utilize the system efficiently, minimizing frustration and maximizing the system’s effectiveness.
DCMC opening direct care non-emergency services is a big step, and it’s crucial to remember that authenticity is key to building trust with patients. Like any brand, a successful transition hinges on demonstrating genuine care and commitment to the community. This means transparent communication and a genuine focus on patient needs, which resonates deeply with patients and builds a strong reputation, just as authenticity is essential to brand building suggests.
Ultimately, focusing on genuine care will help DC’s transition to direct care thrive.
Patient Interface Features
The patient portal provides a streamlined experience for accessing and managing their health information. Key features include secure online scheduling, viewing medical records, communicating with providers, and requesting prescription refills. These functionalities enhance patient engagement and autonomy in their healthcare journey.
- Online Scheduling: Patients can schedule appointments, view available slots, and modify appointments directly through the patient portal, eliminating the need for phone calls in many cases. This feature improves scheduling efficiency and reduces wait times.
- Secure Messaging: Patients can communicate with their providers through a secure messaging system within the portal. This feature fosters better communication and allows for timely follow-up on questions and concerns.
- Record Access: Patients can access their medical records, including lab results, diagnoses, and treatment plans, improving transparency and enabling proactive health management.
- Prescription Refills: Patients can request prescription refills conveniently through the system, streamlining the process and reducing potential delays.
Provider Interface Features
The system’s provider interface is designed for efficient clinical workflows. Key functionalities include secure access to patient records, electronic prescribing, secure messaging with patients, and integration with other healthcare systems.
- Electronic Health Records (EHR) Access: Providers have secure access to comprehensive patient records, including medical history, diagnoses, and treatment plans. This provides a holistic view of patient care.
- Electronic Prescribing: The system supports electronic prescribing, which improves efficiency and reduces errors associated with manual prescribing.
- Secure Communication with Patients: Providers can securely communicate with patients via the system, enabling timely follow-up and improved patient engagement.
- Integration with Other Systems: The system integrates with other healthcare systems, ensuring data consistency and interoperability.
Technical Aspects of System Functionality
The DirectCare system leverages a robust server infrastructure and secure communication protocols to ensure data integrity and confidentiality. It utilizes a web-based platform for accessibility across various devices and operates on a cloud-based architecture, enhancing scalability and reliability. Data encryption and access controls are implemented to protect sensitive patient information.
“The system employs industry-standard encryption protocols to safeguard patient data.”
Functionality Overview
| Functionality | Patient | Provider |
|---|---|---|
| Scheduling | View available appointments, schedule appointments, modify appointments | Manage appointment bookings, view schedules |
| Messaging | Communicate with providers | Communicate with patients |
| Record Access | View medical records | Access patient records |
| Prescribing | Request prescription refills | Prescribe medications electronically |
| Billing | View billing statements | Process billing information |
Addressing Potential Issues

Navigating a system transition, especially one as significant as shifting from DCMC to DirectCare, inevitably presents potential challenges. Understanding these issues and proactively developing solutions is crucial for a smooth and successful transition. Addressing potential problems head-on can prevent larger, more complex issues from arising and ensure a positive experience for patients and staff.The transition from DCMC to DirectCare involves significant changes in processes, systems, and technologies.
Identifying potential obstacles early on allows for the development of robust mitigation strategies, ultimately minimizing disruptions and maximizing efficiency.
Potential System Glitches
Early identification and proactive resolution of system-related issues are paramount. Problems like login failures, data transfer errors, or application crashes can disrupt workflow and negatively impact patient care. Robust testing procedures, including thorough system checks, stress tests, and user acceptance testing, can uncover potential glitches and ensure system stability during the transition. Developing a comprehensive troubleshooting guide, readily accessible to all staff, is critical for swift resolution of technical problems.
Patient Concerns and Conflicts
Patients may have anxieties and concerns regarding the transition to DirectCare. These concerns might range from uncertainties about access to care to apprehensions about the new system’s functionality. Establishing clear communication channels, including dedicated help lines and FAQ pages, is essential for addressing patient concerns. Regular updates and transparent communication about the transition process can help alleviate anxiety and foster trust.
Conducting surveys to gather patient feedback can provide valuable insights into the effectiveness of communication strategies and allow for timely adjustments to address evolving concerns.
Staff Training and Support
Comprehensive training programs are essential for equipping staff with the necessary skills and knowledge to effectively utilize the DirectCare system. Addressing questions and concerns proactively during training sessions and offering ongoing support are crucial for smooth system integration. Mentorship programs and peer-to-peer support networks can further enhance staff understanding and reduce friction during the transition period. Providing ongoing training modules and resources can maintain the competency of staff throughout the transition period.
Switching from DCMC to open direct care non-emergency care is a big step, and it’s exciting to see how this change can improve access to vital services. Thinking about the impact on our communities, especially when considering initiatives like the work of sustaining our waters the fox wolf watershed alliance , it’s clear that responsible healthcare practices are crucial for a healthy environment and well-being.
Ultimately, streamlining DCMC to open direct care will help us better serve the needs of patients in a more accessible and efficient way.
Escalation Procedure
A well-defined escalation procedure is vital for promptly resolving critical issues. This procedure should clearly Artikel the steps for reporting and addressing problems, ensuring that issues are not overlooked or allowed to escalate further. A tiered approach, with designated contacts for different levels of issues, ensures prompt attention and resolution.
- Tier 1: Initial point of contact for minor issues. This might involve a dedicated help desk or a designated staff member. A quick resolution for minor issues is paramount to maintaining productivity and minimizing delays in patient care.
- Tier 2: Handles issues that require specialized expertise or are more complex. This tier might involve IT support staff or designated system administrators.
- Tier 3: For critical issues that significantly impact patient care or system functionality. This involves senior management, IT management, or relevant department heads. This tier prioritizes immediate solutions and ensures that the issue does not cause long-term problems.
Illustrative Case Studies
Real-world examples of transitioning from a legacy system (like DCMC) to a new, more efficient system (like DirectCare) provide valuable insights. Understanding how these transitions unfolded, the challenges encountered, and the eventual outcomes can help us anticipate and mitigate potential issues during our own implementation. This section will explore hypothetical and real-world cases, highlighting the key steps involved and lessons learned.
Hypothetical Case Study: “The Riverview Clinic”
The Riverview Clinic, a small, rural practice, is migrating from its outdated DCMC system to the more modern DirectCare platform. The transition involved several key phases: initial data migration, staff training, and ongoing system monitoring. The clinic implemented a phased rollout, beginning with a select group of providers and gradually expanding coverage to the entire staff. A dedicated project team was established to manage the process, including a point of contact for resolving technical issues and user support.
Steps Involved in the Transition
The Riverview Clinic’s transition included the following key steps:
1. Needs Assessment: A detailed evaluation of the current DCMC system and identification of specific needs for the DirectCare system. This included determining which data points needed migration and what functionalities were essential for the clinic.
2. Data Migration Planning: A comprehensive plan for migrating patient data, ensuring accuracy and completeness.
This involved creating a robust data mapping strategy and identifying potential data inconsistencies.
3. Staff Training and Support: Rigorous training sessions for all staff to familiarize them with the DirectCare system. This included hands-on practice and a dedicated help desk for addressing questions and issues.
4.
System Testing and Validation: Thorough testing of the DirectCare system, including data validation, workflow testing, and user acceptance testing, to confirm that it meets the needs of the clinic.
5. Phased Implementation: A gradual implementation process that started with a smaller subset of staff and gradually expanded to the entire clinic, allowing for adjustments and feedback.
6. Post-Implementation Monitoring: Ongoing monitoring of the DirectCare system to identify and resolve any issues that may arise.
This included gathering feedback from staff and patients.
Real-World Example: “The Evergreen Health System”
The Evergreen Health System, a large multi-location healthcare provider, successfully migrated from a legacy DCMC system to DirectCare. Their approach involved a robust project management structure, a well-defined communication strategy, and dedicated training resources. They established clear roles and responsibilities for each team member, and ensured timely communication and support to all stakeholders. The transition was supported by significant IT infrastructure upgrades to facilitate the data migration and system integration.
Summary of Case Studies
| Case Study | Patient Outcomes | Lessons Learned |
|---|---|---|
| Riverview Clinic (Hypothetical) | Improved patient access, reduced administrative burden, enhanced data accuracy. | Phased implementation and robust training are critical for successful transitions. Prioritize data validation to avoid errors. |
| Evergreen Health System (Real-world) | Enhanced efficiency in patient care, improved operational workflow, and enhanced data security. | Comprehensive planning, strong project management, and clear communication channels are essential for large-scale transitions. |
Last Point: Dcmc To Open Directcare Non Emergency Care
In conclusion, the transition from DCMC to DirectCare Non-Emergency Care presents a substantial evolution in healthcare accessibility. By understanding the procedures, potential issues, and security measures, patients and providers can confidently embrace this new system. This guide has provided a comprehensive overview, offering a practical roadmap for successful integration and a more patient-centric healthcare experience.