Upgrading for Quicker Community Care
Upgrading to provide better quicker care to the community is crucial for ensuring everyone has access to high-quality healthcare. This initiative looks at the current state of healthcare in our community, pinpointing areas needing improvement and proposing practical strategies for a better, more accessible system. We’ll delve into community needs, current delivery models, and explore innovative solutions for a healthier future.
We’ll examine various factors influencing healthcare access, from demographics to infrastructure. A deeper look at best practices in similar communities and successful initiatives will provide valuable insight. Ultimately, this discussion aims to lay a foundation for a more responsive and effective healthcare system, ultimately benefiting every member of our community.
Defining Community Needs
Understanding the diverse needs of our community is crucial for developing effective healthcare solutions. A comprehensive approach requires recognizing the specific requirements of various demographic groups and identifying potential disparities in access to quality care. This analysis will help us tailor our services to meet the unique needs of every member of our community.
Healthcare Access and Satisfaction Factors
Healthcare access isn’t simply about proximity to facilities. It encompasses affordability, availability of services, cultural competency of providers, and the overall patient experience. Factors like transportation, language barriers, and insurance coverage significantly impact access and satisfaction. Community perceptions of healthcare providers and institutions play a vital role as well. Trust and communication are essential for positive patient outcomes.
Community Member Categories and Their Needs
Different community members have varying healthcare needs. Understanding these differences allows us to tailor our services to meet individual requirements. For example, children have distinct needs compared to seniors, and each group requires specialized care. The needs of vulnerable populations, such as those with low incomes, disabilities, or limited English proficiency, must be addressed through targeted interventions.
Moreover, the specific healthcare needs of immigrant populations must be considered, especially regarding language barriers and cultural sensitivities.
Identifying Potential Disparities
Disparities in healthcare access exist within many communities. These disparities often stem from socioeconomic factors, geographical location, and individual circumstances. For example, individuals in rural areas might face challenges in accessing specialized care, while low-income individuals may struggle with affordability. Access to preventative care and chronic disease management may also differ significantly across demographic groups.
Factors Influencing Healthcare Access and Satisfaction
Several factors influence both access to and satisfaction with healthcare services. These include the availability of transportation, the affordability of care, the cultural sensitivity of healthcare providers, and the overall quality of the healthcare facilities. Additionally, communication barriers and the availability of culturally appropriate services can influence both access and satisfaction. The physical environment of healthcare facilities also plays a role in patient experience.
Comparative Analysis of Demographic Groups, Upgrading to provide better quicker care to the community
| Demographic Group | Specific Healthcare Needs | Potential Access Disparities | Influencing Factors |
|---|---|---|---|
| Children | Pediatric care, vaccinations, preventative screenings, mental health support | Limited access to specialized pediatric services in rural areas, lack of affordable childcare during appointments | Geographic location, affordability of care, availability of childcare |
| Seniors | Chronic disease management, geriatric care, medication management, mental health support for aging | Limited access to transportation, difficulty navigating complex healthcare systems, lack of support services for seniors living alone | Age-related physical limitations, social isolation, cognitive decline, affordability of care |
| Low-income individuals | Affordable care, access to preventative services, mental health support, chronic disease management | High cost of care, lack of insurance coverage, limited access to transportation | Poverty, lack of insurance, limited financial resources |
| Individuals with disabilities | Specialized care, accessible facilities, communication support, mental health support | Lack of accessible facilities, communication barriers, lack of culturally appropriate care | Physical limitations, communication challenges, lack of support systems |
| Immigrant populations | Culturally competent care, language assistance, understanding of specific health concerns, access to culturally appropriate services | Language barriers, lack of trust in healthcare system, lack of knowledge of healthcare system | Language barriers, cultural differences, limited knowledge of the healthcare system, potential lack of documentation |
Evaluating Current Healthcare Delivery
The community’s healthcare system is a complex web of interconnected components, each playing a vital role in ensuring the well-being of its residents. Understanding the current state of healthcare provision, identifying strengths and weaknesses, and comparing it to best practices in similar communities is crucial for developing a plan to enhance access and quality of care. This assessment provides a framework for evaluating the current healthcare infrastructure and resources, paving the way for targeted improvements.The current healthcare system, while serving the community, faces challenges in accessibility, efficiency, and resource allocation.
A critical examination of its strengths and weaknesses, coupled with a comparison to best practices in similar communities, will highlight areas requiring attention. This evaluation considers the existing infrastructure and resources, ultimately informing strategies for a more effective and comprehensive healthcare delivery system.
Current State of Healthcare Provision
The current healthcare system in the community is a mix of public and private facilities. Public hospitals are often understaffed and facing increasing patient loads, while private clinics may have limited capacity or geographic reach. This uneven distribution can lead to disparities in access to care, particularly for underserved populations.
Strengths of the Current System
The system’s strengths lie in its existing network of primary care physicians and community health centers. These facilities are often highly accessible and provide a first point of contact for many residents. Furthermore, local hospitals maintain robust emergency departments, ensuring immediate care for critical situations.
Weaknesses of the Current System
Several weaknesses exist, including the limited availability of specialized care, such as cardiology or oncology services. Waiting times for appointments and procedures are often excessive. A lack of coordination between different healthcare providers also hinders the delivery of comprehensive care. There are also reports of inadequate mental health services, creating a significant gap in the overall healthcare provision.
Comparison with Best Practices in Similar Communities
Neighboring communities with comparable demographics and socioeconomic profiles demonstrate more efficient healthcare systems. These communities often have integrated healthcare networks, facilitating seamless care transitions between different providers. They also prioritize preventive care, leading to better health outcomes and reduced long-term healthcare costs. Further, they show a greater emphasis on technology integration, enhancing communication and data management.
Current Healthcare Infrastructure and Resources
The current healthcare infrastructure in our community is diverse. A variety of healthcare facilities, including hospitals, clinics, and community health centers, operate within the system. However, the availability of resources, such as specialized equipment, skilled personnel, and funding, varies significantly across different facilities.
Healthcare Infrastructure Capacity and Limitations
| Facility Type | Capacity | Limitations |
|---|---|---|
| Public Hospitals | High patient volume, but limited capacity for specialized services. | Understaffing, aging equipment, and limited access to advanced technologies. |
| Private Clinics | Varied, dependent on size and specialization. | Limited geographic reach, uneven access to specific specialties, and varying levels of technology. |
| Community Health Centers | Relatively high accessibility and patient volume. | Limited resources, particularly for specialized services, and possible understaffing in some areas. |
Strategies for Improvement: Upgrading To Provide Better Quicker Care To The Community

Improving healthcare delivery requires a multifaceted approach that considers community needs, current challenges, and potential solutions. A crucial step involves developing practical strategies for upgrading services, ensuring better and quicker care for everyone. This requires a commitment to innovation, community engagement, and leveraging technology.The key to effective healthcare improvement lies in understanding the specific needs of the community.
This involves gathering data, analyzing existing systems, and identifying pain points. By identifying these areas of weakness, we can develop targeted solutions that address the specific problems, leading to more efficient and effective healthcare delivery.
Potential Strategies for Upgrading Healthcare Services
A range of strategies can be employed to enhance healthcare services. These strategies should be adaptable to the specific context of each community, ensuring relevance and effectiveness. They should also be measurable and accountable.
- Streamlining Administrative Processes: Implementing efficient systems for appointment scheduling, insurance verification, and billing can significantly reduce wait times and improve patient experience. This includes utilizing online portals and automated systems for administrative tasks. Examples include using electronic health records (EHRs) for efficient data management and reducing the need for redundant paperwork.
- Expanding Access to Primary Care: Increasing the availability of primary care physicians and other healthcare providers in underserved areas can reduce the burden on specialists and emergency rooms. This includes establishing mobile clinics or partnerships with community centers to provide more accessible care.
- Promoting Telehealth Services: Utilizing telehealth platforms for remote consultations, monitoring, and education can increase access to care, especially for patients in rural areas or those with mobility limitations. Examples include remote patient monitoring for chronic conditions, allowing for early intervention and better management.
- Investing in Community Health Workers: Employing community health workers who are familiar with the local community can improve outreach and provide culturally sensitive care. These workers can act as liaisons between patients and healthcare providers, ensuring that care is accessible and tailored to the specific needs of the community.
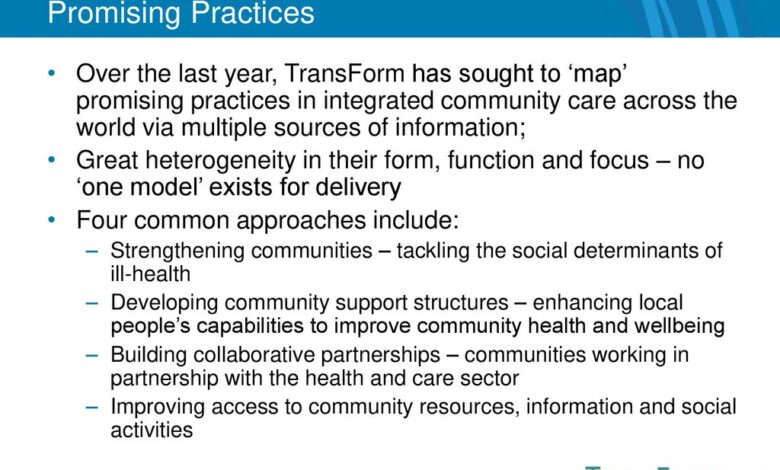
Examples of Successful Community-Based Healthcare Improvement Initiatives
Many successful community-based initiatives have demonstrated the positive impact of targeted interventions. These examples can serve as models for future endeavors.
- The “Healthier Neighborhoods” program in [Example City]: This program focused on improving access to healthy food options and increasing physical activity in low-income neighborhoods, demonstrating a clear link between community well-being and health outcomes.
- The “Community Health Centers” network in [Example State]: This network of centers provided comprehensive primary care services to underserved populations, emphasizing preventative care and health education. This demonstrates the value of localized, community-focused healthcare provision.
Technological Advancements in Healthcare
Technological advancements offer significant potential for improving healthcare delivery. The integration of technology can streamline processes, improve patient outcomes, and increase efficiency.
- Electronic Health Records (EHRs): EHRs allow for secure, accessible patient data, facilitating better coordination among healthcare providers and improving the quality of care.
- Artificial Intelligence (AI): AI can assist in diagnostics, predict potential health risks, and personalize treatment plans, leading to more accurate and timely interventions.
- Wearable Technology: Wearable devices can track vital signs and provide real-time health data, enabling proactive monitoring and early detection of potential health issues.
Community Engagement in Healthcare Improvement
Engaging the community is crucial for improving healthcare delivery. Involving local residents in decision-making processes ensures that the healthcare system meets their specific needs and preferences.
| Strategy | Description | Expected Outcomes |
|---|---|---|
| Community Forums and Town Halls | Organizing meetings to gather feedback and insights from community members on healthcare priorities. | Increased awareness, better understanding of community needs, and identification of potential solutions. |
| Partnerships with Community Organizations | Collaborating with local groups to provide health education and outreach programs. | Improved access to care, increased community engagement, and enhanced health literacy. |
| Patient Advisory Councils | Creating groups of patients who represent the community to provide feedback on healthcare services. | Enhanced patient experience, improved service delivery, and a greater sense of ownership. |
Resource Allocation and Prioritization
Optimizing healthcare resource allocation is crucial for delivering high-quality, timely care. Effective prioritization ensures that limited resources are directed towards the most pressing community needs, maximizing their impact and improving overall health outcomes. This section details the framework for allocating resources, prioritizing needs, identifying funding sources, and outlining associated costs.
Resource Allocation Framework
A robust resource allocation framework should be adaptable and responsive to evolving community needs. This involves a multi-faceted approach, considering factors like the prevalence of specific health conditions, access to care disparities, and the effectiveness of different interventions. The framework should include a clear process for collecting data on community health status, analyzing trends, and projecting future needs. A key element is ensuring transparency in the decision-making process, enabling stakeholders to understand the rationale behind resource allocation decisions.
Prioritizing Community Needs
Prioritization of healthcare needs is essential for maximizing the impact of limited resources. A framework for prioritization should consider the severity and prevalence of health issues within the community. Factors such as the number of individuals affected, the potential for morbidity and mortality, and the cost-effectiveness of interventions should be factored into the decision-making process. For instance, a community experiencing a significant increase in cases of chronic respiratory illnesses might warrant a higher priority for investment in preventative measures and improved access to respiratory care.
Funding Sources for Infrastructure Upgrades
Securing adequate funding is critical for upgrading healthcare infrastructure. Potential funding sources include government grants, philanthropic donations, private investments, and community fundraising initiatives. Government grants are often available for projects addressing specific health needs, while philanthropic organizations may focus on supporting innovative approaches to healthcare delivery. Private investments, particularly in well-defined and profitable ventures, can also contribute significantly.
Cost Analysis of Upgrade Options
Understanding the costs associated with various upgrade options is paramount for effective resource allocation. This analysis should include the cost of new equipment, personnel training, facility renovations, and ongoing maintenance. For example, upgrading an existing clinic to include a dedicated cardiac care unit may involve significant costs for specialized equipment, staff recruitment, and facility modifications. Realistic cost estimations should be developed to ensure projects are financially sustainable.
Summary of Resource Allocation Strategies
| Healthcare Need | Priority Level | Resource Allocation Strategy | Estimated Funding Source | Estimated Costs |
|---|---|---|---|---|
| Chronic Disease Management | High | Expanding preventative care programs, community health workers, and support groups. | Government grants, private donations, community fundraising. | $500,000 – $1,000,000 (initial investment). |
| Mental Health Services | Medium | Expanding mental health clinics, providing mobile mental health services, and increasing access to mental health professionals. | Government grants, private donations, partnerships with mental health organizations. | $250,000 – $500,000 (initial investment). |
| Maternal and Child Health | High | Improving access to prenatal care, increasing the number of birthing facilities, and expanding pediatric care services. | Government grants, private foundations, community fundraising. | $1,000,000 – $2,000,000 (initial investment). |
Measuring Impact and Outcomes
Assessing the success of upgraded healthcare services hinges on meticulously designed metrics. Quantifiable improvements in service delivery, coupled with demonstrable enhancements in community health outcomes, provide concrete evidence of the program’s effectiveness. This crucial step allows for continuous refinement and adaptation to optimize the healthcare system’s performance and address evolving community needs.
Defining Success Metrics
To effectively gauge the impact of upgrading healthcare services, a comprehensive set of metrics must be established. These metrics should reflect the specific goals and objectives Artikeld in the previous phases, focusing on both the immediate improvements in service delivery and the long-term effects on community health. This ensures a holistic evaluation that considers the multifaceted aspects of the upgrade.
Upgrading our services to deliver better, faster care to the community is a top priority. We’re constantly looking at ways to improve, and a recent initiative, like exploring the potential of new technologies, is crucial. This involves a deep dive into various aspects, from user experience to technological integration. In fact, a recent blog post, focusing on the fundamental building blocks of successful projects, is very relevant to this process: Hello world!.
Ultimately, this is all about providing the best possible care to our community members, ensuring their needs are met efficiently and effectively.
- Service Delivery Metrics: These metrics concentrate on aspects like wait times, appointment scheduling efficiency, access to specialists, and the overall patient experience. Shorter wait times and streamlined appointment scheduling contribute to improved patient satisfaction and reduce the stress associated with seeking care. For example, a reduction in average wait time for primary care appointments from 30 minutes to 15 minutes indicates a significant improvement in service delivery efficiency.
Another example is an increase in the percentage of patients who schedule appointments online, demonstrating a shift towards more convenient access to care.
- Community Health Outcome Metrics: These metrics focus on measurable improvements in the health of the community, such as reductions in specific chronic disease rates, improved immunization rates, and lower rates of preventable hospitalizations. For instance, a decrease in the incidence of childhood asthma or an increase in the percentage of the population receiving recommended vaccinations reflects positive community health outcomes.
Quantifiable Improvements in Healthcare Delivery
Demonstrating tangible improvements in healthcare delivery is vital for showcasing the upgrade’s effectiveness. Data-driven evidence, such as reduced patient wait times, increased access to specialists, and improved patient satisfaction scores, clearly articulates the program’s impact.
- Reduced Wait Times: A significant reduction in wait times for various services, from initial contact to specialist appointments, suggests improved efficiency and responsiveness. This translates to better patient experience and timely access to necessary care.
- Increased Access to Specialists: Greater access to specialists allows patients to receive timely and specialized care. This can be measured by tracking the number of appointments scheduled with specialists per month or the proportion of patients able to see a specialist within a specified timeframe.
- Improved Patient Satisfaction: Surveys measuring patient satisfaction can provide valuable insights into the overall experience of receiving care. High satisfaction scores indicate that the upgrade has positively impacted the patient experience.
Measuring Improvements in Community Health Outcomes
Evaluating community health outcomes is crucial to assessing the broader impact of the upgrade. Monitoring key health indicators, such as chronic disease rates, immunization rates, and hospital readmission rates, allows for a comprehensive evaluation. A decrease in these indicators indicates improved community health outcomes.
- Chronic Disease Rates: Tracking the prevalence of chronic diseases, like diabetes and hypertension, can highlight improvements in community health. A decrease in these rates reflects the success of preventive care and management strategies.
- Immunization Rates: Monitoring immunization rates for various preventable diseases, such as measles and influenza, demonstrates the effectiveness of public health initiatives and the community’s participation in preventive measures.
- Hospital Readmission Rates: Lower hospital readmission rates indicate that patients are receiving adequate follow-up care and management of chronic conditions, contributing to improved health outcomes.
Tracking and Reporting on Impact
A systematic process for tracking and reporting the impact of upgrades is essential for ongoing monitoring and adaptation. Regular reporting ensures transparency and accountability, allowing for informed decision-making and resource allocation.
- Data Collection: Regular collection of data on key metrics, using standardized tools and protocols, is essential for effective tracking and reporting. This data collection should include patient demographics, wait times, appointment scheduling, and outcomes of care.
- Regular Reporting: Scheduled reporting, whether weekly, monthly, or quarterly, allows for ongoing monitoring of progress and facilitates timely interventions if needed. These reports should be accessible to relevant stakeholders.
- Data Analysis: Data analysis is essential to identify trends and patterns, enabling proactive measures to address challenges and celebrate successes. Data visualization techniques can be used to present complex information in an easily understandable format.
Metrics for Measuring Success
This table summarizes the metrics used to evaluate the success of upgrading healthcare services.
| Metric Category | Metric | Target/Goal | Measurement Method |
|---|---|---|---|
| Service Delivery | Average wait time for appointments | 15 minutes | Tracking appointment scheduling data |
| Service Delivery | Percentage of online appointments | 75% | Tracking appointment scheduling data |
| Community Health Outcomes | Rate of childhood asthma | Decrease by 10% | Reviewing public health records |
| Community Health Outcomes | Immunization rates (e.g., MMR) | 95% | Reviewing immunization records |
Future Considerations and Sustainability
Sustaining the improvements in our community’s healthcare delivery requires a proactive approach that considers potential challenges and proactively develops sustainable models. The journey towards enhanced care isn’t a sprint; it’s a marathon demanding ongoing adaptation and resourcefulness. We must be prepared to navigate unforeseen obstacles and ensure the long-term viability of the upgraded system.
Potential Challenges to Maintaining Improvements
The upgraded healthcare system, while designed for efficiency and improved access, is susceptible to several challenges. Funding fluctuations, staffing shortages, and technological obsolescence are key concerns. Adapting to evolving community needs and maintaining a skilled workforce are crucial. Technological advancements and their integration into the system will also need continuous evaluation. Unexpected increases in the prevalence of specific diseases or health conditions could also strain the resources of the upgraded system.
Developing Sustainable Models for Long-Term Care Delivery
Developing sustainable models requires a multifaceted approach. Financial stability is paramount. Exploring diversified funding streams, including partnerships with private organizations and community fundraising initiatives, is essential. This could include exploring innovative financing mechanisms like community health trusts or impact bonds. Furthermore, optimizing resource allocation through efficient inventory management and streamlined processes is critical.
Training and development programs for healthcare professionals are vital to maintain a skilled and adaptable workforce. A focus on preventative care and community health initiatives will also contribute to long-term cost-effectiveness and sustainability.
Continuous Improvement and Adaptation to Evolving Needs
Continuous improvement and adaptation are key components of long-term sustainability. Regular assessments of community health needs are crucial for identifying emerging trends and adapting services accordingly. Public health data should be used to anticipate and address potential health crises and challenges. Data-driven decision-making is essential for ensuring the upgraded system remains responsive to the community’s needs. Regular audits of service delivery and quality control measures are essential to identify areas for improvement and prevent issues from escalating.
Long-Term Sustainability of the Upgrade
The long-term sustainability of the upgrade hinges on several factors. A comprehensive financial plan, including contingency funds and diverse revenue streams, is crucial. Building partnerships with community organizations and stakeholders ensures shared responsibility and broader support. Prioritizing preventative care, coupled with community engagement programs, fosters a healthier population, thus lowering healthcare costs over time. A robust system for evaluating and improving the effectiveness of the upgrade is essential to identify areas needing improvement and adapt to changing circumstances.
Regular training and development opportunities for healthcare professionals will ensure a skilled and adaptable workforce, capable of responding to future needs.
Table of Potential Future Challenges and Solutions
| Potential Future Challenges | Potential Solutions |
|---|---|
| Funding fluctuations | Diversify funding sources (e.g., private partnerships, grants, community fundraising). Implement cost-saving measures without compromising quality. |
| Staffing shortages | Develop competitive compensation and benefits packages. Implement comprehensive training and development programs. Explore alternative staffing models (e.g., telehealth, collaborative care). |
| Technological obsolescence | Establish a technology refresh schedule. Implement a plan for incorporating new technologies. Invest in ongoing training for staff on new technologies. |
| Evolving community needs | Conduct regular community health assessments. Develop flexible service delivery models. Prioritize preventative care and health promotion initiatives. |
| Increased prevalence of specific diseases | Develop contingency plans to address potential surges in demand. Enhance the capacity of diagnostic and treatment facilities. |
Summary
In conclusion, upgrading to provide better quicker care to the community isn’t just about improving healthcare; it’s about fostering a healthier and more equitable community for everyone. By addressing current shortcomings, embracing innovative solutions, and prioritizing resource allocation, we can build a sustainable healthcare system that meets the evolving needs of our community. This process requires ongoing evaluation, adaptation, and community engagement to ensure long-term success.